L9 - K Okkenhaug - Tolerance Flashcards
(27 cards)


why is tolerance important?
(2)
avoid responding to self materials
avoid responding to innoculous substances
is tolerance aquired or hard wired?
aquired
Strong adaptive immune responses almost always require the antigen to be injected in,….
Strong adaptive immune responses almost always require the antigen to be injected in a mixture known as an adjuvant
how do adjuvants work?
- cue an infection is taking place
- convert soluble protein into particular material
- which can be ingested by APC (eg macrophage)
what is actually in adjuvant?
Many of them contain bacterial products, which stimulate macrophages or dendritic cells through Pattern Recognition Receptors. Complete Freund’s Adjuvant (CFA) for example, contains ground-up mycobacteria.
describe central tolerance? for t cells
- T cells:
- Negative selection leads to deletion of those T cells with strong affinity for self
describe central tolerance ofr B cells
since need activating by T cells - shouldnt need tolerating
B cells that react to abundant antigens on self cells are eliminated as they develop. Self-reactive cells have an opportunity to avoid apoptosis by replacing the light chain in a process called receptor editing. High doses of soluble proteins result in anergy rather than apoptosis.
what is anergy?
A state of immune unresponsiveness
why isnt central tolerance enough?
thymus doesnt present all self antigens
so we have peripherla tolerance too
Some antigens are not expressed until after the immune system has matured
what is AIRE
a transcription factor called AIRE, which turns on many ‘peripheral’ genes in the thymus, so that the developing T cells may be exposed to their products.
allows thymus to express most peripherla proteins for tolerance to be calibrated againstq
what happens in individuals which lack AIRE
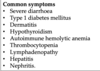
suffer from a wide range of autoimmune conditions. The condition is called APECED, autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy.
4 proposed mechanisms for peripheral tolerance?
- ignorance
- split tolerance
- anergy
- Suppression
describe split tolerance?
since immune pathways are interdependant - dont all need tolerising.
ie, since B cells rely on T cells, if T cells are tolerised - thats enough
The explanation of this is that it takes 100-1000- times more antigen to tolerise B cells than it does T cells. As a result, this type of split tolerance situation is reasonably common for self serum proteins.
describe what Anergy is - as an explanation for peripheral tolerance
an be induced in T cells if the receptor is engaged by the MHC molecule but the second signal is absent
constantly occurs wiht self proteins.
Large amounts of soluble antigen lead to anergy if it is not cross-linked at the cell surface.
what is meant by supression - peripheral tolerance wise
Idea that Treg can supress the activation of T cells bound to self antigens on MHC II - supress proliferation
secretion of IL-10 and TGF beta
Regulatory T cells express high levels of CTLA-4 - which binds B7 more strongly
not too sure on this one tbh
what is IPEX
- X linked
- congenital lack of Treg
- mutations in FOXP3
- die under age of 2 unless given bone marrow transplant
- shows peripheral tolerance is essential
what is meant by ignorance? - peripheral tolerance
when potentially self-reactive T cells are not activated. This could be because antigens are hidden from the immune system in locations that are not freely exposed to surveillance. These immunologically privileged sites include the brain, eye and testis.
CTLA-4 and PD-1 are ……
CTLA-4 and PD-1 are inhibitory receptors that antagonise T cell activation and co-stimulation
give some facotrs which affect tolerance
timing, dose of antigen, amount of costimulation and location
does tolerance only operate in early loife?
no - bone marrow transplants can lead to the host developing a chimerism - which is needed to allow grafts to be accepted
check the notesa dn read ofr this one
why dont mothers reject their babies?
- Physical barrier to the mother’s T cells.
- Lack of MHC class I expression on trophoblasts. Trophoblast cells that form the outer layer of the placenta in contact with maternal tissues do not express classical class I molecules and so are not targets for cytotoxic T cells.
- Production of immunosuppressive factors such as -fetal protein and IDO (indoleamine 2,3-dioxygenase, a tryptophan catabolising enzyme).
describe a co-receptor blockade?
CD28 costimulation is essential - blocking blocks immune repsonse.
Abetacept (soluble CTLA4 fusion protein) blocks CD28
use to treat rheumatoid arthritis and to prevent graft rejection.
can anti-PD1 and Canti-CTLA4 antibodies be used in cancer therapy?
yep - they blockimmune check points - allowing cancers new neopeptides (cancer mutations make self peptides different) to look foreign - elciting an immune repsonse.



