Lab 2: Blood Circulation Flashcards
(168 cards)
Blood Pressure: Definition
Normal Blood Pressure Range
“will you be so kind to specify under which conditions and where?”
question:
“What is the blood pressure in the temporal artery?”
Answer:
“I can not say specifaclly because i do not know your systemic pressure. i can make an estimaion based on the fact that you look healthy and by using the approximite distance of the temporal artery from your heart.”
Systolic BP definition
Systolic: The highest pressure anywhere (where there is a pulsation) during the cardiac cycle
Siastolic BP Definition
Diastolic: The lowest arterial pressure during the relaxation of the left ventricle
Cardiac Output Definition
Volume of blood pumped from each ventricle per minute
CO equations

Stroke Volume: definition, equations, factor that affect it

What factors influence blood pressure (scheme)?

Preload definition:
- The extent to which heart muscle fibers are stretched before the onset of systole
- This depends greatly on the end-diastolic ventricular volume (EDV): volume load created by blood entering ventricles at end of diastole before contraction
- It is not possible to measure preload in vivo, but we can use the EDV as an indicator
Factors affecting Preload
**add

Afterload Definition
•The extent to which heart muscle fibers are stretched during systole/ejections
…The ressistance ventricles must overcome during systole
Factors affecting Afterload

Frank-Starling Law: definition
Definition: a law that describes the relationship between end-diastolic volume and cardiac stroke volume
- Cardiac contractility is directly related to the wall tension of the myocardium.
An increase in end-diastolic volume (preload) will cause the myocardium to stretch (↑ end-diastolic length of cardiac muscle fibers), which increases contractility (↑ force of contraction) and results in increased stroke volume in order to maintain cardiac output.
This relationship between end-diastolic volume and stroke volume is shown in the Frank-Starling curve.
Aim: maintain CO by modulating contractility and SV
↑EDV= ↑STRECH= ↑CONTRACTILITY= ↑SV= ↑CO

Diffrence in systemic and pulmonary circulation: pressure, resistance, compliance

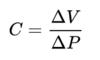
Compliance Deffinintion:
?
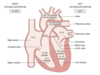
Geeral stages of the cardiac cycle

When and why do the hears valves open?

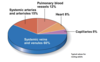
Relative proportion of blood volume throughout the cardiovascular system:
What is Pressure Pulse:
is the difference between the systolic and diastolic pressures.
Pulse pressure = P(systolic) - P(diastolic)
■ The most important determinant of pulse pressure is stroke volume. As blood is ejected
from the left ventricle into the arterial system, arterial pressure increases because
of the relatively low capacitance of the arteries. Because diastolic pressure remains
unchanged during ventricular systole, the pulse pressure increases to the same extent
as the systolic pressure.
■■ Decreases in capacitance, such as those that occur with the aging process, cause
increases in pulse pressure
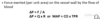
Mean Arterial Pressure
■■ is the average arterial pressure with respect to time.
■■ is not the simple average of diastolic and systolic pressures (because a greater fraction
of the cardiac cycle is spent in diastole).
■■ can be calculated approximately as diastolic pressure plus one-third of pulse pressure.
* to know the exact vaule we must do an integral of the graph (area under the graph)

Ejection Fraction deffinition:

What is arterial compliance?
Compliance is the ability of a hollow organ (vessel) to distend and increase volume with increasing transmural pressure
* In compliance, an increase in volume occurs in a vessel when the pressure in that vessel is increased. The tendency of the arteries and veins to stretch in response to pressure has a large effect on perfusion and blood pressure. This physically means that blood vessels with a higher compliance deform easier than lower compliance blood vessels under the same pressure and volume conditions.[1] Venous compliance is approximately 30 times larger than arterial compliance.[2] Compliance is calculated using the following equation, where ΔV is the change in volume (mL), and ΔP is the change in pressure (mmHg):
Windkessel effect
Windkessel effect is a term used in medicine to account for the shape of the arterial blood pressure waveform in terms of the interaction between the stroke volume and the compliance of the aorta and large elastic arteries (Windkessel vessels) and the resistance of the smaller arteries and arterioles.

Distribution of blood flow ( as a % of CO)
..