M1 Techniques Flashcards
Clinical features of DMD
- Enlargement of calf, gluteal, deltoids
- LL muscles more affected
- Between 6-11 yrs old, strength decreases linearly
Causes of DMD
- Lack of dystrophin protein
- Affects DGC/SGC
- Dystrophin also responsible for signalling
What are mdx/dko mice?
- Mdx mice → muscular dystrophy x-linked
- Dko mice → double knock-out mice (Utrophin KO as well)
- More severely affected
- Complete loss of integrity across ribcage
Difference b/w muscles of the mdx and wild-type mice
- Muscles of the mdx mice are larger than wild-type mice
- But they are producing similar force
- ∴ Intrinsically → mdx mice produce less force per cross-sectional area and are more fragile (as they lack dystrophin)
Pre-clinical evaluation of efficacy of drugs: 1) Whole body functional tests
- Non/minimally invasive tests
- Overall health or functional capacity
- Assess/monitor treatment → tracks performance
- i.e. running/swimming/climbing
- But generally no definitive (accurate) and provides non-specific measurements of muscle groups
a) WBFT: Vertical Hang test
- Latency-to-fall on to a padded mat
- Assess overall muscular strength and endurance
- Pro:
- Natural exercise
- Simple to perform/evaluate (↑reliability)
- Assess motivational/volitional aspects too
- Cons:
- Can’t assess specific muscles
- Crude assessment of strength and endurance
b) WBFT: Roper rod
- Spinning wheel → see how long it takes for mice to fall
- Evaluate muscle fatigue and motor performance
- Pro:
- Simple, non-invasive
- Able to track performance regularly
- Provides assessment of coordination, motivation, fatigue
- Cons:
- Difficult to identify specific muscle
c) WBFT: Grip strength
- Mice holds onto the bar while being pulled on its tail
- Basic assessment of strength
- Able to screen drug for fast or delayed response
- Pro:
- Simple, non-invasive
- Assess regularly and track
- Con:
- Crude measure
- Difference between skills of investigators (Someone who knows how to hold the animal compared to someone who doesn’t)
- Biomechanical advantage (i.e. hunchback) can affect how well the animal holds on, and thus affect reliability
2) In vitro/situ/vivo measurements
- Able to look at drug effects on specific muscles
- Able to assess structure and function of the muscles (including fatigue and damage)
- Measure speed of contraction and relaxation
a) In vitro
- Muscle out of animal
- Pros:
- Assess functional parameters of muscles directlySp
- Free from influence of nerve or blood supply
- Cons:
- Less physiological give nerve and blood supply are removed
- Need to ensure all motor units activated for accuracy of force measurements (technical issues)
b) In situ
- Nerve and blood supply intact
- Pros:
- Able to preserve N and BS → able to stim isolated nerve to muscles
- Able to assess properties of single muscle and its specific adaptations to interventions
- Cons
- More technically challenging
- More time consuming: limited number of preparations that can be assessed
c) In vivo
- Pros
- Can be done in minimally invasive manner
- Whole muscle group of muscles assessed
- Use for training/conditioning programs in controlled manner
- Cons
- More technically difficult
- Equipment can be expensive
- Not isolated to specific muscle
3) Cellular levels
- Cellular levelsMechanically skinned fibres
- Studies E-C coupling/SR release/SR reuptake
- Chemically permeabilised fibres
- Study speed of shortening, damage to fibres
Pros and cons of cellular levels
- Pros:
- Study cellular level for mechanistic understanding
- Cons
- Technically difficult
- Requires expensive equipment
Importance of diaphragm
- Function of diaphragm can be a good assessment of drug interventions
Other essential analysis
- Not only the structure-function of the muscle is important for assessment
- Assess complementary histological, immunohistochemical, biochemical
- CK levels
- Other pathways: i.e. protein syn vs BD
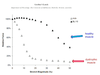
Are dystrophic mice more susceptible to contraction-induced injury?
- Sarcolemmal fragility of mdx mice (i.e. seen from evans blue dye infiltration)
- Greater susceptibility to rupture after shock and stretch
- Compromised costomere → impaired dissipation of force → ↑risk of injury
- Incidence of high muscle fibre branching also contributes to susceptibility
What happens when membrane integrity is compromised?
- ↑ Influx on Ca → necrosis/proteolysis of muscle proteins
What are contraction clots
- Area of hypercontractility, loss of integrity where fibres are damaged at these points
5 theories for muscle fibre necrosis
*My Cat’s Going Very Indie*
- Mechanical hypothesis
- Calcium hyothesis
- Gene regulation hypothesis
- Vascular hypothesis
- Inflammatory hypothesis
1) Mechanical hypothesis
- Loss of DGC leads to contraction-induced rupture of muscle cell membranes → accumulation of serum proteins
- Exercise in DMD patients and mdx mice → greater muscle damage than unaffected controls
2) Calcium hypothesis
- Influx of Ca into cell → overwhelming cell ability to buffer the change
- Overexpress of calpain/caspases
3) Gene regulation hypothesis
- Failure of molecules localising to the membrane when DGC is absent → prevent proper signalling molecules recruited
4) Vascular hypothesis
- Disruption is membrane proteins → loss of NO signalling → muscles being ischemic and thus cannot repair
- nNOS KO mice do not have muscle disease → nNOS may play a direct role


