Medically Relevant Bacteria - Gram Negative Curved and Cooccobacilli-LM Flashcards
(36 cards)
This is a gram neg, curved rod bacteria with a single polar flagellum. It is a non lactose fermenter but ferments glucose. What is it from this discription and the pictures

Vibrio Cholerae
How is vibrio cholerae transmitted
- Usually a disease of poor sanitation (water with human fecal contamination)
- Large dose is required to produced disease due to acid in stomach killing organisms
V cholerae is a non invasive enterotoxogenic bacterium that produces a potent enterotoxin choleragen? how does it work?
- A domain controls its biologic activity
- A1 peptide enzymatically transfers ADP-ribose from NAD to a GTP regulatory protein which leads to activation of adenylate cyclase and the overproduction of cyclic AMP
- B domain binds the toxin to cellular receptors (GM1 receptor)
How would you Dx cholerae?
Rx?
- Dx- voluminous “rice water stool” presumptive for cholera
- Gram stain stool to see organism or
- Isolation using V. Cholera selective thiosulfate-citrate-bile salts-sucrose (TCBS) agar
- Rx – fluid and electrolyte replacement, doxycycline can shorten disease course

A gram neg, curved rod, is a non lactose fermenter, motile,
•Ingestion of contaminated water, milk or undercooked foods (raw clams) causes.
What is it?

Campylobacter jejuni
How does campylobacter jejuni infection progress?
- Enteroinvasive and after 2-4 day incubation get acute enteritis (fever, loose bloody diarrhea, nausea and abdominal pain)
- Generally self-limiting but may last a week
- Relatively small inoculum is required to cause illness
For C. jejuni, how would you…
DX
RX
?
- Dx - Gram stain may reveal curved (“seagull” or “comma”) shaped organisms, culture at 5% O2, 10% CO2, 85% N2 at 42°
- Rx – early erythromycin treatment may shorten disease course
This picture is showing a gram neg,bacteria that is a non lactose fermenter.
•Lives in the mucus layer above the gastric epithelium and produce urease (buffered from acid)
What in the picture is characteristic of its name?

Helical shape
Helicobacte pylori
H pylori transmits feco-oral or oral-oral; what other conditions is it associated with?
How does it cause these?
- Associated with chronic gastritis, gastric and duodenal ulcers, gastric adenocarcinoma and gastric MALT lymphoma
- Down regulation of somatostatin-producing D cells leads to elevated gastrin levels and enhanced acid secretion
- Chronic superficial gastritis → atrophic gastritis → adenocarcinoma
What would you use to Dx H pylori? think about the fact is produces urease.
Rx.
Breath urea test was highlighted but
- Stool antigen test, urease test on biopsy, breath urea test, IgG serology, visualized microscopically, cultured on chocolate agar in a microaerophilic environment
- Rx – PPI, clarithromycin, and amoxicillin, or metronidazole (clarithromycin-based triple therapy) or a PPI or H2RA, bismuth, metronidazole, and tetracycline (bismuth quadruple therapy)
These are obligate anaerobes so they like to live in abcesses, most encapsulated, non lactose fermenter, gram neg bacilli or cocco bacilli? Does the picture help? What are they?

Bacteroids and prevotella
These are all opportunistic with immunosuppression but B fragilis has what virulence factor?
Dx?
Rx?
Anti-phagocytic capsule
- Dx - Gram stain and ANAEROBIC culture
- Rx frequently resistant to many antibiotics and local antibiotic susceptibility patterns are needed as well as antibiotic sensitivity of the patient’s cultured organism
- Debride necrotic tissue, drain pus
Where are Prevotella sp. found?
What can they cause?
Prevotella sp. are similar to, and previously classified as, bacteroides
- Part of the normal oral and vaginal flora
- Can cause obstetric and gynecologic infections, aspiration pneumonia, chronic otitis media and sinusitis, and abscesses in lung, oral cavity, brain abscesses, and human bite wounds
This is a picture of a gram neg coccobacilus, aerobic, non-motile, aquatic. First ID the organism then tell me what is significant about what it produces?
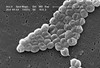
Acinetobacte baumannii
Produces B-lactamase
How does acinetobacter baumannii present?
Dx
Rx
- Nosocomial infections or immunocompromised patients
- Commonly colonizes irrigating and INTRAVENOUS solutions (so can go almost anywhere in body)
- Respiratory tract, CSF, peritoneal fluid, urinary tract infections
- Dx – culture
- Rx – amikacin, minocycline (intrinsically resistant to cephalosporins, macrolides, and penicillins and developing resistance to carbapenems)
Haemophilus is a gram neg coccobacilli whose capsule is a major virulence factor. It is spread by direct contact (day care centers)
What are the types of haemophilus that we learned about?
What type of people must be vaccinated?
Influenzae
Influenzae Type B
Ducreyi
Parainfluenzae
aegypticus
ASPLENIC
How does H influenzae present?
What is special about type B?
•Pneumonia, acute epiglottitis, bacteremia, meningitis, septic arthritis, cellulitis, otitis media, purulent pericarditis, endocarditis, arthritis and osteomyelitis
- H. influenzae type b - most common cause of bacterial meningitis in children 6 months-2 years
- Unencapsulated strains produce ear, sinus and respiratory infections (usually chronic smokers, alcoholics or elderly)
What is this

Chancre caused by H ducreyi.
Will also cause this ( painful, unilateral); its called bubbos by the way.

H parainfluenzae,
H aegypticus presentation
pneumonia endocarditis;
conjunctivitis
H. Parainfluenza Dx
Rx
Prevention
- Dx -Gram stain of CSF, capsular antigen detections, culture is fastidious (10% CO2 required) and organisms require factors X (hemin) and/or V (NAD) in media (present in chocolate agar), PCR
- Rx –IV or parenteral third generation cephalosporin
- Prevention – 3 doses of one of the following: MONOVALENT Hib VACCINE, quadrivalent Hib vaccine (Hib + DTP), pentavalent Hib vaccine (Hib + DTP + hepatitis B)
Gram neg coccobacilli that is encapsulated and a strict aerobe? The main one is also called whooping cough, what is it.

Bordetella pertussis- spread by direct contact

What are the exotoxins that Bordetella produces?
- Filamentous hemagglutinin: involved in attachment to host cells
- Pertussis Toxin: adp-ribosyl-transferase that interferes with G-protein signals from cell surface receptors (A subunit) and involved attachment to respiratory epithelia and mφs (B-subunit)
- Invasive adenylate cyclase toxin: increases cAMP, inhibiting immune effector cell functions
- Tracheal cytotoxin: causes ciliostasis and loss of ciliated epithelial cells
- Lethal (dermonecrotic) toxin: heat stable and causes tissue destruction
Whooping cough has stages of the disease can you describe them
Catarrhal
Paroxysmal
Convalescent
- Highly contagious laryngotracheobronchitis usually seen in infants
- 7-14 day asymptomatic incubation period
- Catarrhal stage - fever, rhinorrhea and a highly infectious cough
- Paroxysmal phase - spasmodic “whooping” cough that may last 6 weeks with posttussive vomiting and lymphocytosis accompanied by minimal granulocytosis
- Convalescent phase - secondary complications may occur (encephalopathy, seizures and pneumonia)
Bordetella pretussis Dx
Rx
Prevention
- Dx – clinical symptoms, PCR, grown on Bordet-Gengou agar media, and serologic testing
- Rx – erythromycin can shorten disease course
- Prevention – DTaP vaccine x 5 followed by Tdap( this is important) in adulthood (acellular pertussis not as protective as pre-1997 whole cell preparations DTwP)






