Meningitis Flashcards
(87 cards)
What is meningism?
Triad of:
- Headache
- Photophobia
- Neck rigidity
What is meningitis?
https://www.youtube.com/watch?v=gIHUJs2eTHA
Usually inflammation of the meninges
What is the pathophysiology behind bacterial meningitis?
https://www.youtube.com/watch?v=xQC6L8M6XfU
Inflammation of the meninges, usually result of infection
Involves at least five steps:
- Attachment to mucosal epithelial cells
- Transgression of the mucosal barrier
- Survival in the blood stream
- Entry into CSF
- Production of overt infection in the meninges +/- brain infection (encephalitis).
What are the 3 layers of the meninges (from outermost to inner most)?
- Dura Mater
- Arachnoid Mater
- Pia Mater

What is normally the cause of death in meningitis?
Sepsis - not the actual meningeal inflammation
What routes do organisms reach the meninges by?
Either by:
- Direct extension from the ears, nasopharynx, cranial injury or congenital meningeal defect
- Haematogenous spread.
What are the main causes of meningism?
- Meningitis
- Sub-arachnoid Haemorrhage
- Malignancy
- Autoimmune disease
When assessing neck stiffness, what key finding would indicate meningeal irritation?
Stiffness on flexion. If on rotation, more likely to be caused by cervical problem like spondylosis
What are bacterial causes of meningitis?
- Neisseria Meningitidis
- Streptococcus pneumoniae (pneumococcus)
- E. coli
- Group B streptococci
What other conditions can mimic meningitis?
- Cervical spondylosis
- Cervical fusion
- Parkinson’s disease
- Raised ICP - esp if there is impending tonsillar herniation.
- Acute dystonic reaction
- Tetanus
What are viral causes of meningitis?
- Enteroviruses
- Echoviruses
- Parechoviruses
- Coxsackie A and B
- Poliovirus
- Mumps
- Herpes simplex virus
What are the most common causes of bacterial meningitis in neonates (<1 month)?
- E. Coli and other coliforms
- Group B Strep
- Listeria Monocytogenes
What are the most common causes of bacterial meningitis in 3 month to 6 year olds?
- Nisseria Meningitidis
- Streptococcus Pneumoniae
- Haemaphilus Influenzae
- Group A strep.
- Staph. aureus
What are the most common causes of bacterial meningtis in those over the age of 6?
- Neisseria Meningitidis
- Strep. Pneumoniae
Which patient groups is listeria meningitis more common in?
- Immunocompromised
- Neonates
- Over age of 50
What are symptoms seen in meningitis in adults?
- Headache
- Irritability
- Stiff neck
- Photophobia
- Fever/Rigors
- Altered level of consciousness
- Vomiting
- SEIZURES
What fungi can cause meningitis?
- Cryptococcus neoformans
- Candida albicans
What are symptoms of meningitis in a child/neonate?
Can be vague symptoms:
- Lethargy
- Malaise
- Vomiting
- Poor feeding
- Irritability
What ENT problems can lead to meningitis?
- Otitis Media
- Sinusitis
What signs can present in meningitis?
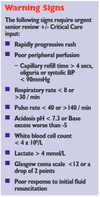
- Pyrexia
- Tachycardia
- Signs of shock - cool peripheries, decreased BP
- Cranial nerve palsies
- Petechial Rash
- Kernig’s Sign
- Brudzinski’s Sign
- Jolt accentuation
- Opisthotonos
What is jolt accentuation?
Rapid horizontal rotation of the neck (2–3 Hz) in a patient with suspected meningeal irritation results in exacerbation of pre-existing headache.
Rotational and centrifugal forces upon inflamed meninges are thought to exacerbate cephalgia when meningeal irritation is present.
What is Brudzinski’s Sign?
With the patient in the supine position, passive neck flexion results in active hip flexion and knee flexion.

What is thought to be the mechanism behind brudzinski’s Sign?
Passive neck flexion results in mechanical stress on the spinal nerves and the arachnoid mater, which may be somewhat alleviated by active hip flexion and knee flexion. When the subarachnoid space is inflamed, as with meningitis, mechanical forces on the arachnoid mater result in tenderness and an attempt to alleviate pain (hip flexion, knee flexion)

What is Kernig’s Sign?
https://www.youtube.com/watch?v=YgRX3IUaaeE
With the patient lying supine with the hip flexed to 90°, the examiner attempts to passively extend the knee from 90°. Resistance to passive knee extension at less than 135° is considered a positive sign.