Microbiology (All Topics) Flashcards
(276 cards)
Respiratory infections:
Outline the main features of Pneumonia and Bronchitis
Pneumonia:
- Mortality is 5 to 10%
- 20 to 40% are hospitalised
- 30 to 50% are Commuinity Acquired Pneumonia (CAP)

Respiratory infections:
Outline the symptoms and microscopitc findings of:
- S.Pneumonia
- H.Influenza
- M.Catarrhalis
- S.Auerus
- K.Pneumonia

Respiratory infections:
Outline the symptoms and features of:
- Legionella pneumophilia
- Mycoplasma pneumonia
- Chlamydia pneumonia
- Chlymydia psittaci
- Bordatella pertussis
- TB
- Coxiella Burnetti
Coxiella Burnetti:
- Domestic/farm animals
- Aerosol
- Diagnose with serology
- Treat with macrolides
Macrolide > Clarithromycin
Tetracycline > Doxycyline

Respiratory infections:
Outline the resipiratory tract infections associated with:
- HIV
- Neutropenia
- Bone Marrow transplant
- Splenectomy
- Cystic fibrosis

Respiratory infections:
Outline the daignosis of respiratory tract infections

Respiratory infections:
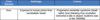
Outline the Antibiotics used for Community (Classical and Atypical) and Hospital Aquired Pneumonia

Respiratory infections:
What is the simplistic antibiotic framework for respiratory tract infections?
To simplify:
Just Gram positive:
- Amoxicillin
- Flucloxacillin
- Vancomycin
Mostly Gram positive, little gram negative:
- Coamoxiclav
- Cefuroxime
Clearly both:
- Cafotaxime
- Meropenem or Piperacillin & Tazobactam
Mostly Gram negative, little gram positive:
- Ciprofloxacin
Just Gram negative:
- Cefazidime
- Gentamicin
Atypical Pneumonia:
- Clarithromycin/doxycyline

PUO & Fever in the returning traveller
What is the definition of Pyrexia of Unknown Origin?

PUO & Fever in the returning traveller
- What is the approach to Neutropenic fever?
- What are the other key points to consider in PUO?

PUO & Fever in the returning traveller
What are the main causes of fever in the returning traveller?

PUO & Fever in the returning traveller
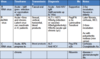
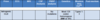
What are the Severity & Liver stage, Length of Rhythm, Blood film and treatment of P.Malaria

PUO & Fever in the returning traveller
What are the symptoms, investigations and management options for Typhoid?
Antibiotics:
- Cotrimidazole, Chloramphenicol or ampicillin
- (Multi-drug resistance) >> 3rd gen cephalosporin or azithromycin

PUO & Fever in the returning traveller
What are the Severity & Liver stage, Length of Rhythm, Blood film and treatment of P.Vivax

PUO & Fever in the returning traveller
What insect carries malara?

PUO & Fever in the returning traveller
What are the Severity & Liver stage, Length of Rhythm, Blood film and treatment of P.Ovale
P.Malaria

PUO & Fever in the returning traveller
What are the Severity & Liver stage, Length of Rhythm, Blood film and treatment of P.Falciparum

PUO & Fever in the returning traveller
What are the major features of sever or complicated Malaria?
IS PHARAOS:
- I: Impaired concoiusness/Seizures
- S: Shock
- P: Pulmonary oedema or ARDS
- H: Hypoglycaemia (<2.2mmol)/Haemoglobinueria
- A: Anaemia (Hb <8)
- R: Renal imapairement
- A: Acidosis (ph <7.3)
- O: Other indications
- S: Spontaneous bleeding/DIC

PUO & Fever in the returning traveller
What are the investigations for P.Falciparum?

PUO & Fever in the returning traveller
What is the treatment for P.Falciparum?

PUO & Fever in the returning traveller
What are the common signs of P.Falciparum?

PUO & Fever in the returning traveller
What are the symptoms of P.Falciparum?
Uncommon signs:
DDACC
- Diarrhoea
- Dark Urine
- Abdrominal pain
- Confusion
- Cough

PUO & Fever in the returning traveller
What is the definition of Classical PUO and give some examples
PUO Definition:
>38.3⁰C fever on several occasions persisting >3/52 without diagnosis despite >1/52 of intensive Ix

PUO & Fever in the returning traveller
What is the definition of Healthcare associated PUO and give some examples

PUO & Fever in the returning traveller
What is the definition of Neutropenic PUO and give some examples