Microvascular complications of diabetes mellitus Flashcards
(36 cards)
What does poor diabetes control increase the risk of?
Microvascular AND macrovascular complications
What are some sites of microvascular complications? What do they cause
- Retinal arteries → retinopathy
- Glomerular arterioles → nephropathy
- Vasa nervorum → neuropathy
- Vasa vasorum = small blood vessels which supply the nerves
NOTE: -pathy = damage
What are the risk factors for microvascular complications?
- Severity of hyperglycaemia
-
Hypertension
- The higher the SBP, the higher the risk of microvascular complications
- NOTE: There is a link between hypertension and diabetes - they often co-exist
- Genetic predisposition
-
Hyperglycaemic memory
- This refers to the phenomenon where prolonged exposure to hyperglycemia can epigenetically modify gene expression
- This effect is sustained even after hyperglycemic control is therapeutically achieved
- Therefore, patients who had poorly controlled diabetes at some point, even if their blood sugar levels are controlled now, are at an increased risk of microvascular complications
Describe the mechanism of how hyperglycaemia can lead to microvascular complications.
- Hyperglycaemia and hyperlipidaemia leads to hypoxia and oxidative stress
- This activate inflammatory signalling cascades, leading to local activation of pro-inflammatory cytokines and hence inflammation
- Inflammation causes damage to organs
Important pathways to remember
What are some important things to remember about diabetic retinopathy?
- Main cause of visual loss in people with diabetes
- Main cause of blindness in people of working age
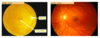
What would a normal retina look like when looking through a fundoscope?
- Optic disc - more medial (nasal)
- Macula - more lateral (temporal)
- Macula involved in visual acuity (central vision) and colour vision
- Lots of blood vessels
What are the 4 types of retinopathy?
- Background diabetic retinopathy
- Pre-proliferative diabetic retinopathy
- Proliferative retinopathy
- Maculopathy
What would background diabetic retinopathy look like when looking through a fundoscope?
- Hard exudates
- Yellow flecks - cheese colour
- This is due to leakage of lipid contents from the retinal blood vessels
- Microaneurysms
- Red dots
- This is due to localised dilation (bulging) of the micovessel vessel walls
- Blot haemorrhages
- The microaneurysms can rupture and leak blood
If untreated, this leads to pre-proliferative diabetic retinopathy

How is background diabetic retinopathy managed?
- Improve control of blood glucose
- Warn patient that warning signs are present
What would pre-proliferative diabetic retinopathy look like when looking through a fundoscope?
- Cotton wool spots (also called soft exudates)
- These represent retinal ischaemia
- EXTRA:
- Ischaemia → hypoxia → blockage of axoplasmic flow (as this requires energy) → deposition of intra-axonal organelles (these are the cotton wool spots that we see)
If untreated, new vessels will grow → proliferative retinopathy
NOTE: Axonal transport = a cellular process responsible for movement of substances (e.g. organelles) to and from the cell body, through the cytoplasm of its axon (i.e. axoplasm)

What would proliferative retinopathy look like when looking through a fundoscope?
There are visible new vessels on the optic disc or elsewhere in the retina
- NOTE: Mechanism
- Significant amount of retinal BVs already damaged (due to microaneurysms → haemorrhages etc.)
- This leads to the body releasing a growth hormone which stimulates the formation of new blood vessels to try and restore blood supply to the retina
- However these blood vessels are weaker, which can cause problems

How is pre-proliferative and proliferative diabetic retinopathy managed?
Panretinal photocoagulation
- Laser therapy
- Laser beams fired into retina to destroy the ischaemic tissue
- Reduced area of ischemic tissue reduces the stimulus for new blood vessel formation (neovasacularisation)
- The point of this is not to improve vision as vision will already be poor due to the ischaemia
-
But you want to prevent the condition from getting even worse
- You want to prevent the formation of new blood vessels as this is what causes problems
What would maculopathy look like when looking through a fundoscope?
- Same disease as background diabetic retinopathy
- BUT this time near the MACULA
- Hard exudates near macula
- Because the problem is near the macula, it’s more likely to cause damage to the macula than a problem elsewhere in the retina
- This can threaten direct vision

How is maculopathy managed?
Only needs a GRID of photocoagulation
- NOT panretinal photocoagulation
- There is only a problem around the macula
- So you only need treatment (photocoagulation) there - not the whole retina

What are the features of diabetic nephropathy?
Presents with:
- Hypertension
- Progressively increasing proteinuria
- Progressively deteriorating kidney function
- Classic histological features
What is a dangerous consequence of diabetic nephropathy?
Presence of diabetes and CKD increases the risk for cardiovascular events
What are the 3 types of histological features to look at in diabetic nephropathy?
- Glomerular
- Vascular
- Tubulointerstitial
What histological glomerular changes will be seen in diabetic nephropathy?
- Mesangial expansion
- Basement membrane thickening
- Glomerulosclerosis
- Scarring of the glomerular capillaries (meaning loss of functional filtration tissue)
Mesangium:
- Essentially a supporting framework which forms between the glomerular capillaries
- Made up of:
- Mesangial cells
- Extracellular matrix

COME BACK Describe the pathophysiology of diabetic nephropathy (online and Laz)
Describe the epidemiology of diabetic nephropathy in diabetes.
Type 1
- 20-40% after 30-40 years
Type 2
- Probably equivalent to T1DM but epidemiology affected by certain factors
- Age at development of disease (i.e. of T2DM)
- Racial Factors
- Age at presentation of T2DM
- Loss (i.e. most deaths) due to cardiovascular morbidity??
What are the ranges of proteinuria?
- Normal Range: <30mg/24hrs
- Microalbuminuric Range: 30 - 300mg/24hrs
- Assymptomatic Range: 300 - 3000mg/24hrs
- Nephrotic Range: >3000mg/24hr
These ranges represent the amount of urine found in the urine
COME BACK What are the strategies for intervention or management of diabetic nephropathy?
- Diabetes control
- Blood pressure control
- Inhibition of the activity of RAS system
- EXPLAIN THIS
- Stopping smoking
- Smoking stimulates oxidative stress because of increased formation of reactive oxidative species
What is the most common cause of neuropathy?
Diabetes
- Therefore diabetes is the most common cause of lower limb amputation
What does neuropathy result from?
Neuropathy results when the vasa nervorum get blocked
- Vasa nervorum = small blood vessels which supply the nerves


