MOD F TECH 47 Extremes of Body Temperature Flashcards
(24 cards)
Extremes of Body Temperature
•Normal body temp
–36.9°C
–
•Abnormally low body temp
–Hypothermia
–
•Abnormally high body temp
–Hyperthermia
- Heat Exhaustion
- Heat Stroke
Hypothermia
•is a lowering of the body core temperature below 35°C
•
•Heat may be lost in 4 ways:
–Convection – carried by moving air
–Conduction – passing onto a solid object
–Radiation – dissipating into surrounding air
–Evaporation – through evaporation of water from skin or wet clothing
Hypothermia
3 classifications
1.Acute Hypothermia = immersion hypothermia were person looses heat very quickly e.g. falling in cold water
●
2.Subacute Hypothermia = Hill walkers who becomes exhausted and unable to generate body heat.
●
3.Chronic Hypothermia = heat loss occurs slowly over days usually. Elderly or homeless
Causes of hypothermia
•Cold environment - unheated room
•
•Exposure to cold weather
•
•Immersion in cold water
•
•Inadequate clothing or diet
Hypothermia
•Risk groups:
–The elderly – live alone, inadequate heating & food, immobility
–Young babies - no thermal regulator especially premature –
no shivering reflex
–People involved in outdoor activities in Winter
–Water Sports even in Summer
–Alcoholics
–Chronic Illness
Hypothermia
Hypothermia in adults
- Slow heart rate <40 may be undetectable
- Skin ice cold to touch
- Pale, peripheral cyanosis, appears dead - moribund
- Dilated pupils, unreactive
- Breathing slow, shallow, undetectable
- Reducing LOC, slurred speech
- Visual disturbance
- Irrational behaviour
- Stumbling
- Collapse
Hypothermia - Management
- ABC’s
- Handle gently!
- Administer O2 aiming for 94% - 98%
- Wrapping patient enough to prevent further heat loss and moving to a warm environment
- Allowing the body to recover gradually
- Giving hot drinks if the patient is fully conscious and uninjured
- Check blood sugars
- Remove to Hospital
DO NOT….
•
–Strip clothing unless wet and in vehicle
–Give alcohol
–Rub the patient’s skin
Wrap cold patients in foil blankets
In cardiac arrest:
•Defibrillation is not likely to be effective if the patient’s core temp. <30oC
•
•If with clinician – attempt one loop of defibrillation/drugs then BLS only
•
•DON’T STOP RESUSCITATION IN THE FIELD
Hypothermia in babies
- Remember that babies have not got fully developed reflexes so may not shiver even when very cold….
- Pale, unwell appearance
- Unwell, not crying, no appetite, no interest in surroundings
- Cold to touch
Management
- Hazards ABCD
- Cover the baby to prevent further heat loss
- Warm baby gradually
- Suspect hypothermia in all cases of near drowning.
- Dilated pupils, undetectable pulse, minimal respiration.
- Commence & maintain resuscitation
•Suspect hypothermia in all cases of near drowning.
•
•Dilated pupils, undetectable pulse, minimal respiration.
•
•Commence & maintain resuscitation
Resuscitation
They’re not dead until they’re warm and dead!!
Local Cold Injury - Frostbite
- Can be superficial (close to surface of skin) or deep
- Normally involves exposed areas – fingers, ears, nose etc.
- Comes on slowly and is generally not painful
- Skin may be white / waxy, feels numb
- As thawing occurs, area looks mottled blue and patient experiences a hot stinging sensation
- Blisters may develop within a few hours
Frostbite - Treatment
- Get out of the cold
- Rewarm the injured part with body heat
- Cover any blisters with a dry, sterile dressing
Do not
Rub or massage a frost bitten area
Rub snow on a frostbitten part
Apply ointments
Apply tight bandages
Allow a thawed extremity to refreeze
Handle a frostbitten extremity roughly
Hyperthermia
- Heat Exhaustion
- Heat Stroke
Effects of Extreme Heat
•In extremely hot conditions, the body’s heat loss mechanisms may fail.
•
- When the atmospheric temperature equals the body temperature, it becomes impossible for the body to lose heat by radiation. If there is also high humidity (when the air is laden with moisture), sweat does not evaporate well.
- In these circumstances, particularly during strenuous exercise when extra heat is generated by muscular activity, heat exhaustion, or the more dangerous condition, heatstroke, may develop.
Hyperthermia
•Heat Exhaustion (38 °C)
–Caused by excessive sweating combined with inadequate water intake
–
•Heat Stroke (40 °C)
–Occurs as body starts to dehydrate resulting in
- Hypothalamus breaking down
- Body continuing to produce heat with no means of cooling, in effect overheating
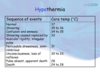
Heat Exhaustion & Heat Stroke
Overheating = loss of body fluids and salts.
Heat exhaustion progresses to heat stroke - an acute medical condition with high mortality rate.
Heat exhaustion
- Usually develops gradually and is caused by loss of water and salt from the body by excessive sweating accompanied with inadequate fluid intake
- More common in people who are
unaccustomed to working or exercising in
a hot, humid environment, and in those
who are unwell, especially with
diarrhoea and vomiting.
•Heat is still being produced but the body
has no way of cooling
•Can often lead to Heat Stroke if not managed early and effectively
People at Risk…
–People working in high temperature environments
–People in the sun for long periods of time
–Excessive physical exertion, for example military personnel exercising, or people who have taken Ecstacy
Hyperthermia – S&S
- Unconsciousness – sudden and deepening
- Initially a rapid and weak pulse, becoming full and bounding
- Shallow breathing, becoming rapid, noisy and panting
- Headaches and dizziness developing into confusion and delirium
- Muscular cramps and twitching
- Initially pallid colour, turning flushed
- Sweating and warm skin, becoming dry and very hot
Signs & Symptoms
Heat exhaustion;
May have flu-like symptoms such as:
- Headache
- Nausea
- Dizziness
- Cramps
- Tachycardia
- Sweaty
Heat stroke;
Neurological symptoms
such as:
- Decreased level of consciousness
- Ataxia
- Convulsions
- Sweating may well be absent
Heat Exhaustion - Management

- ABC’s
- Move to a cool environment
- Place patient at rest
- Cool drinks in small regular quantities
- Sponging with luke warm water
Heat Stroke - Management
- Remove as much clothing as possible
- Wrap in a wet sheet (if available)
- Fanning the patient vigorously
- Placing cold packs under the arms, in the groin area and around the neck
- Treat the patient accordingly if unconscious

Dehydration
Drink before you feel thirsty!

Febrile Convulsions
- Sudden rise in body temperature
- Caused by excessive fever
- Usually affect children up to 3 years
- Parents have usually tried ‘Calpol’ to no avail
- Hazards ABCDE
- Remove child’s clothes
- Clinicians will consider Paracetamol (Calpol)


