Mod9-Obj3&4-Reproductive system: Female Flashcards
(34 cards)
The female reproductive system
- Produce and release gametes
- Nurture a developing fetus
- Give birth
Female reproductive anatomy
The ovary releases ova eggs, which travels into the uterine/fallopian tube. Fimbriae help to drag eggs from the ovary into the fallopian tube as there is a gap between the ovary and the uterine tube.
The uterine tube connects to the uterus, where implantation and development of a baby occurs, connected from the cervix to the vagina, which is connected to the external genitalia

External genitalia
The vulva
- Mons pubis: area over pubic symphysis
- Labia majora: 2 fatty skin folds
- Labia minora: 2 thin, hair-free skin folds
- Clitoris: erectile tissue, richly innervated, sexual arousal
- Vestibule (greater vestibular (bartholin’s) glands: release mucus to lubricate intercourse

Internal genitalia

The female duct system
The vagina, uterus and uterine/fallopian tubes make up the female duct system and provide a passage way for conception and birth
- Not continuous
- There is a gap between the ovaries and the uterine tubes! Some oocytes don’t manage to make it into the tube and are lost in the peritoneal cavity

The vagina provides a passage way to:
Provides a passage way to:
- Eliminate menstrual fluids
- Recieve the penis during intercourse
- Expel fetus during child birth
The vagina
Is a thin-walled tube, 8-10cm long
- Both muscular (smooth muscle) and elastic
- Acidic environment helps keep the vagina free of infection but makes it hostile to sperm
- Teenagers have not yet developed an acidic environment, making them more susceptible to an STD

The uterus is…
A hollow, thick muscular organ that:
- Receives, retains and nourishes offspring
- Consists of the body (major region), fundus (top region) and cervix (joins to the vagina)
- Glands in the mucosa of the cervix secrete mucous that block the spread of bacteria in the uterus from the vagina (also blocks entry of sperm except at midcycle when mucous becomes less viscous)

The uterine wall is composed of 3 layers:
- Perimetrium: outermost layer
- Myometrium: bulky, middle muscular layer (contracts to expel baby)
- Endometrium: Inner, mucosal layer (allows for implantation of the fertilised egg)

The Endometrium (Inner, mucosal layer) is made up of 2 layers:
- Functional layer (stratum functionalis)
* *Undergoes cyclic changes due to ovarian hormones and is shed during menstruation - Basal layer (stratum basalis)
* *Unresponsive to ovarian hormones

What can go wrong with the uterus?
Cervical cancer affects 450,000 women/yr
- Gardasil (vaccine) provides protection from HPV, which induces cancer
The uterus is supported by a number of ligaments, as well as the pelvic floor muscles
Prolapse of the uterus
Stretching and tearing of these ligament and muscles (of the uterus) during childbirth can result in the unsupported uterus sinking down through the external opening of the vagina

The uterine tubes
Also known as the fallopian tubes or oviducts (10cm long)
- Receive ovulated oocytes
- Typical site where fertilisation occurs
- Fimbriae (ciliated) sweep over the ovary to capture the oocyte
- Muscular movements and beating cilia carry the oocyte towards the uterus

Ovaries
2 small organs that:
- Produce female gametes (oocytes)
- Secrete female sex hormones (estrogen & progesterone)
Each ovary consists of the:
- Medulla: inside region which is highly vascularised
- Cortex: Outside region where follicles are matured to release oocytes

Producing Oocytes: Oogenesis
- Occurs in the ovaries
- Begins in the fetal period (by birth a female has a lifetime supply): stays in a suspended state until puberty
- A small number of primary oocytes are recruited each month-one is selected to go through meioses to form the mature ova
- High rate of chromosome error in oogenesis compared to spermatogenesis
Oogenesis
Oogonia multiply by mitosis
- Primary oocytes begin meiosis but stall
- Each month after puberty, a few primary oocytes are activated
- One is selected to resume meiosis 1 (result is two haploid cells (1st polar)
- The secondary oocyte arrests in metaphase II and is ovulated
- If penetrated by sperm the secondary oocyte completes meiosis II, yielding: ovum (functional) and 2nd polar body

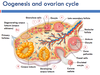
Oogenesis and the ovarian cycle
Theses meiotic events coincide with follicle development in the ovary

Oogenesis and the ovarian cycle diagram
The ovarian cycle: Two phases
Events that mature and egg are called the ovarian cycle
- Follicular phase (d1-14): follicle growth, ovulation at the end of this stage
- Luteal phase (d15-28): Period of corpus luteum activity (nomally 14d)

Follicular phase
- GnRH* released by the hypothalamus stimulates the anterior pituitary gland to release *FSH* and *LH
- FSH stimulate follicle maturation
- FSH stimulates the thecal cells and granulosa cells to secrete estrogens
- Increasing levels of estrogens stimulate a surge in LH secretion which triggers ovulation

Ovulation (step 6)
Bulging follicle eventually ruptures the wall of the ovary and the oocyte is released
- Oocyte surrounded by granulosa cells (corona radiata)
- A number of follicles are being prepared within the ovary at any one time
- Increases in LH (and FSH) signals time for ovulation

Luteal phase
- The LH surge transforms the ruptured folicle into the corpus luteum (CL)
- The CL produces estrogen, progesterone and inhibin
- If fertilisation does not occur the CL degrades and the cycle begins again

Hormonal regulation of ovarian cycle
- Oestrogen and progesterone are released from the ovaries
- Inhibit (and stimulate) hypothalamus to release gonadotrophin releasing hormone (GnRH)
- Acts on the anterior pituitary to release follicle stimulating hormone (FSH) and luteinising hormone (LH)
- feedback loop






