Neoplastic hematopathology Flashcards
(173 cards)
Most common site of extranodal B cell lymphoma
stomach
B cell neoplasm demographics
- Low grade more common in older adults; high grade in kids and young adults
- Most B cell neoplasms have male predominance
- exceptions showing female predominance:
- primary mediastinal lymphoma
- follicular lymphoma
- MALT lymphoma
- exceptions showing female predominance:
- DLBCL > FL > CLL > mantle cell lymphoma
- CLL most common leukemia
CLL/SLL
- genetics
- age
- presentation
- morphology (SLL and CLL)
- immunophenotype
- molecular and cytogenetics
- transformation to
- CLL has strongest genetic influence of all B cell neoplasms
- Familial clustering in 5%
- Risk in 1st degree relatives is 5x baseline
- Median age = 65
- Presentation
- Adenopathy, splenomegaly, PBL and BM involvement
- autoimmunity; positive DAT in 30%
- immunodeficiency; hypogammaglobulinemia in 30-50%
- M protein occasionally
- Morphology
-
SLL
- Diffuse nodal involvement
- small lymphs, occasional prolymphocytes
- proliferation centers; many prolymphocytes (light and dark areas)
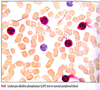
-
CLL
- small lymphs
- prolymphs < 11%
- 11-55% prolymphs = CLL/PLL
- smudged cells in EDTA; not seen in heparin smears
- lymphocyte count > 5 x 109/L (monoclonal B cell lymphocytosis under this number)
- small lymphs
-
SLL
- Immunophenotype
- positive for
- CD19
- CD20 (dim)
- CD22
- CD5
- CD43
- CD23
- sIg (dim)
- CD79a
- CD11c (dim and variable)
- bcl-2
- Negative for
- FMC-7
- CD10
- bcl-6
- CD38 and ZAP-70 expressed in half
- positive for
-
Molecular and cytogenetics
- most common cytogenetic abnormality is trisomy 12
- # 1 FISH abnormality: del 13q (good)
- others: tri 12, del(11q), del(14q), and del(17p)
- 20% have normal FISH
-
Transformation:
- most common form is PLL
- Richter (large cell lymphoma)
- rarely transforms to Hodgkin
CLL prognosis adversely affected by
- B symptoms
- Diffuse pattern of marrow involvement
- peripheral lymphocyte doubling time < 1 year
- high initial lymphocyte count (>30,000)
- unmutated Ig heavy chain gene variable region (IgVH)
- resemble pregerminal center B cells
- likely to progress
- candidates for treatment
- CD38 and ZAP-70 in > 30% of cells correlates with unmutated status
- Chromosomal status by FISH
- Good: normal karyotype or del(13q) only
- Poor: 11q or 17p deletions
Mantle cell lymphoma
- presentation
- morphology
- variants
- immunophenotype
- molecular and cytogentic
- prognosis adversely affected by
- Presentation
- adenopathy
- tends to involve Waldeyer ring and GI tract (lymphomatous polyposis)
- Morphology
- diffuse or vaguely nodular lymph node effacement
- small to medium sized lymphocytes, irregular nuclear contour, small subtle nucleolus
- mitoses frequent
- admixed histiocytes and hyalinized vessels
- neither proliferation centers nor prolymphocytes
- variants: blastoid, pleomorphic, small cell, marginal zonelike
- blastoid composed of large cells with high mitotic rate
- blastoid and pleomorphic more aggressive
- small cell variant resembles SLL; marginal zone like variant resembles MZL
- Immunophenotype
- positive for: CD19, CD20 (bright), CD22, FMC-7, CD5, CD43, sIg (bright), bcl-1 (cyclin D1, prad 1), blc-2
- negative for: CD23, CD11c, CD10, CD99
- Molecular and cytogenetic
-
Positive for t(11;14)
- rearrangment of JH region of IgH (14q32) to the CCND1 (11q13)
- results in cyclin D1 (bcl-1) amplification
- FISH is most sensitive
- most have additional abnormalities, often in chromosome 13
-
Positive for t(11;14)
- Prognosis adversely affected by mitotic rate > 10/HPF and Ki-67 > 40%
Follicular lymphoma
- presentation
- morphology
- grading
- diffuse growth
- FL variants
- in the marrow
- immunophenotype
- molecular and cytogenetic
- prognosis adversely affected by
- Presentation
- isolated lymphadenopathy without constitutional symptoms
- Morphology
- nodular lymphoid proliferation: back to back, fused follicles with attenuated mantles
- often overruns capsule
- follicles lack polarity, tingible body macrophages, plasma cells, and have few mitoses
- 2 cell types: small cleaved cells (centrocytes) and large noncleaved cells (centroblasts)
- Grading
- proportion of centroblasts in 10 fields
- grades 1 and 2 are low grade
- Grade 1: 0-5/HPF
- Grade 2: 6-15/HPF
- Grade 3
- 3A: >15/HPF + some residual centrocytes
- 3B: >15/HPF and no centrocytes
- Diffuse growth
- lack of follicles and dendritic cells by CD21 and/or CD23 IHC
- when low grade, called FL with focal diffuse growth
- when high grade, called DLBCL
- lack of follicles and dendritic cells by CD21 and/or CD23 IHC
- FL variants
-
Intrafollicular FL (FL in situ)
- intact interfollicular zones and open sinuses
- follicles have cytologic features of FL: purely centroblasts and centrocytes that express bcl-2
-
Isolated cutaneous FL
- good px
- lacks CD10 and bcl-2 expression
- bcl-6 positive
- lacks BCL2 rearrangement
-
Isolated GI FL
- good px
- duodenum
- Pediatric FL is usually grade 3
-
Intrafollicular FL (FL in situ)
-
In the marrow
- focal paratrabecular aggregates
- may be discordant with low grade in marrow and high grade in lymph node
-
Immunophenotype
- Positive: CD19, CD20 (bright), FMC-7, CD22, CD10, sIg (bright), bcl-2, and bcl-6
- Negative: CD5, CD43, CD11c, CD23
- Higher grade are less CD10 positive
- Ki-67 <20% in grades 1-2 and >20% in grade 3
- Background FDC express CD21 and CD23
- Molecular and cytogenetic
-
t(14;18)
- FISH is most sensitive
- Rearrangement of BCL2 on 18 with the J region of IgH on 14
- Results in overexpression of bcl-2 protein with antiapoptotic properties
- translocation not unique to FL and is most common encountered in B lineage lymphoma
- bcl-2 overexpression also not unique to FL; bcl-2 overexpression in non-FL usually not associated with t(14;18)
-
t(14;18)
- Prognosis adversely affected by
- higher age, stage, and serum LDH
- bone marrow involvement
- B symptoms
- low performance status
- anemia
Marginal zone lymphoma (MZL)
- presentation
- morphology
- immunophenotype
- molecular and cytogenetic
- Presentation
- Nodal
- Extranodal (MALT)
- Splenic
- Morphology
-
Nodal
- nodular or diffuse proliferation
- small lymphs, rounded to indented nuclei, abundant pale cytoplasm (monocytoid)
- associated with chronic antigenic stimulation
- most common site is GI tract (especially stomach)
- clonal plasma cells often present
-
Extranodal (MALT)
- variably destructive and/or tumefactive proliferation
- monocytoid B cells and clonal plasma cells
- lymphoepithelial lesions
- reactive polyclonal germinal centers can be present
-
Splenic
- expansion of white pulp
- involves splenic hilar lymph nodes often
- liver sinusoids involved
-
peripheral blood involvement
- splenic lymphoma with villous lymphocytes (SLVL)
- resembles HCL but SLVL more likely to
- display nucleoli
- display polar villous projections
-
Nodal
- Immunophenotype
- Positive: CD19, CD20, CD21, CD79A, FMC-7, bcl-2, sIg (IgM)
- Negative: CD5, CD23, CD10, CD103, annexin A1, CD11c
- plasma cells contain monoclonal cytoplasmic light chains
- CD43 is negative generally, but positive in 30% of MALT lymphoma
- Molecular and cytogenetic
- t(11;18) - rearrangement of API2 and MALT1 genes in stomach and lung
- t(14;18) - MALT1-IgH fusion: ocular, parotid, and cutaneous
- t(3;14) - FOXP1-MALT1 in ocular, thyroid, and cutaneous
- t(1;14) in lung and small bowel
- +3 and +18 in all sites
- A monoclonal gammopathy is present in 30-50% of cases
Hairy cell leukemia
- Presentation
- Morphology
- Immunophenotype
- Molecular findings
- Presentation
- neutropenia, monocytopenia, or aplastic anemia
- splenomegaly
- 4:1 male:female
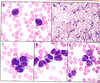
- Morphology
- blood smears
- large lymphoid cells 2x the size of normal lymph
- nuclei round to reniform with smooth contour
- chromatin ground glass with indistinct to absent nucleoli
- hairy projections are circumferential
- Tissue
- Fried egg morphology
- reticulin fibrosis, blood lakes, and mast cells
- in spleen, cells infiltrate the red pulp
- in liver cells are in sinusoids
- Ultrastructure
- ribosome lamellar complexes
- Histochemistry
- cells contain tartrate resistant acid phosphatase (TRAP)
- weak TRAP nonspecific, but strong TRAP staining is specific
- blood smears
- Immunophenotype
- Positive: CD19, CD20, CD22, sIg, CD11C (bright), CD25 (bright), CD103, DBA.44, annexin A1, cyclin D1 (dim, nuclear)
- Negative: CD5, CD43, CD23, CD10
- 10% are CD10+
- No reproducible molecular findings
Prolymphocytic leukemia
- presents abruptly with a very high white count > 100,000/uL, B symptoms, cytopenia, and splenomegaly
- Definition: > 55% prolymphocytes (prominent nucleoli and a moderate quantity of cytoplasm)
Lymphoplasmacytic lymphoma/Waldenstrom macroglobulinemia
- how to diagnose LPL
- how to diagnose Waldentrom
- associated with
- morphology
- molecular and cytogenetics
- Lymphomas wtih plasmacytic features
- SLL/CLL, MCL, and MZL
- LPL diagnosed when these are excluded
- Waldenstrom macroglobulinemia is LPL with an IgM monoclonal gammopathy and marrow involvement
- Associated with HCV and cryoglobulinemia; may respond to anti viral therapy
- Morphology
- small lymphs to plasma cells
- Dutcher bodies possible
- Lymph nodes
- architecture may be normal or effaced
- PAS+ material in sinuses
- Immunophenotype
- Positive: CD19, CD20, CD38, sIg (bright), cIg (plasma cells)
- Negative: CD5, CD23, CD43, CD10
- Molecular and cytogenetic
- t(9;14) involving PAX5 and C region of IgH
Heavy chain disease
- only IgH are produced
- Most common form is alpha H chain disease
- a form of MALT lymphoma also called immunoproliferative small intestine disease (IPSID) or Mediterranean lymphoma, associated wtih C. jejuni
- gamma heavy chain disease (Franklin H chain disease) found in some cases of LPL
- mu heavy chain disease found in some cases of CLL
Diffuse large B cell lymphoma
- presentation
- morphology
- immunophenotype
- molecular and cytogenetic
- prognosis
- Presentation
- rapidly enlarging lymph node or extranodal site
- localized at presentation, bone marrow involvement uncommon (10%)
- Morphology
- diffuse nodal effacement by predominantly large cells (larger than a macrophage nucleus)
- Immunophenotype
- positive: CD19, CD20, CD22, CD45, often bcl-2
- variable: CD10, CD5, and bcl-6
- CD5 expressing cases must be distinguished from blastoid MCL (bcl-1+)
- Ki67 60-99%
- Molecular
- BCL2 and BCL6 rarrangements present in 20-30%
- BCL6 gene, 3(q27), rearranges with variety of partners, commonly t(3;14)
- rearrangements of BCL6 more common in the ABC type
- rearrangement of BCL2, t(14;18), more common in the GCB type
- BCL2 and BCL6 rarrangements present in 20-30%
- Prognosis
- germinal center-like has better response to treatment than activated B cell like (ABC)
- Germinal center-like type:
- CD10+ BCL6+ MUM1 -
- CD10+ BCL6 - MUM1-
- CD10- BCL6+ MUM1-
- Non germinal center type
- CD10 - BCL6+ MUM1+
- CD10 - BCL6- MUM1+
Stepwise evaluation of DLBCL subtypes by IHC
- CD10
- if positive, then it’s GC type
- if negative go to #2
- BCL6
- if negative, then non GC type
- if positive, then go to #3
- MUM1
- if positive, then non-GC
- if negative, then GC type
Primary DLBCL of the CNS
- median age
- location in brain
- presentation
- micro
- FISH results
- median age 60 years
- supratentorial mass with radiographic features that mimic GBM
- may present or recur as intraocular lymphoma
- tumor cells often in perivascular cuffs and express pan B antigens
- most cases have BCL6 rearrangement and overexpress bcl-6; BCL2 rearrangement is rare
T cell/histiocyte rich large B cell lymphoma (TCRBCL)
- median age
- micro
- IHC
- marrow
- median 40 years (children to old age)
- diffuse proliferation of small lymphocytes and histiocytes with scattered large B cells
- Small lymphocytes are a mixture of CD4+ and CD8+ T cells
-
absent are
- CD57+ T cells
- T cell rosettes
- small B cells
- CD21+/CD23+ FDC meshwork
-
absent are
- Large B cells express pan B markers and bcl-6; some are EMA+
- Can be positive for CD10
- negative for CD15, CD30, and EBV
- Involves marrow as paratrabecular lymphoid aggregates
Primary mediastinal (thymic) large B cell lymphoma
- gender, age
- micro
- IHC
- molecular
- young adult women, F:M = 2:1
- a sclerosing lymphoma with large B cells entrapped within bands of sclerosis
- Positive: CD45, CD19, CD20, CD79a, CD30
- NEGATIVE FOR surface Ig, CD10, CD5
- Altered MAL gene, gains in 9p (locations of JAK2)
- No rearrangement of BCL2 or BCL6
ALK+ large B cell lymphoma
Rare; immunoblastic/plasmablastic cells that express ALK
Plasmablastic lymphoma
- IHC
- patient population
- site of involvement
- rare; immunoblastic/plasmablastic cels
- Positive: CD38, CD138, IRF4/MUM1, cIg, EBV
- Negative: CD45, CD20, CD56 (in contrast to plasmayctoma)
- Found in HIV+ adults and arises mostly in extranodal sites such as oral cavity mucosa
Intravascular large B cell lymphoma
- aka
- symptoms
- aka angioendotheliomatosis, angiotropic lymphoma, and intravascular lymphomatosis
- symptoms related to small vessel obstruction by large B cells
- lymph node involvement rare
Primary effusion lymphoma
- associated with
- presentation
- micro
- IHC
- Associated with HHV8 and HIV
- Presents with effusion (pleural, pericardial, peritoneal)
- contains large B cells with immunoblastic/plasmablastic/anaplastic morphology and cytoplasmic vacuolization
- negative for B/T/myeloid antigens (CD20, CD79, CD19, CD10, CD3, CD5, CD13, CD14, CD33)
- Positive for CD45, CD30, CD38, CD138, EMA, HHV8
Leg type primary cutaneous DLBCL
rare; affects elderly women
EBV+ DLBCL of the elderly
- affects what population
- other EBV positive large B cell neoplasms
- rare; affects elderly Asian adults
- Other EBV+ large B cell neoplasms
- plasmablastic lymphoma
- PEL
- lymphomatoid granulomatosis
- DLBCL associated with chronic inflammation
- EBV+ DLBCL of the elderly
- EBV+ DLBCL, NOS
Lymphomatoid granulomatosis
- Large B cells destructively invade vessel walls resembling vasculitis
- many reactive T cells, plasma cells, histiocytes
- granulomas are uncommon
- most commonly affects lungs, upper aerodigestive tract, brain, kidneys, and liver
- associated wtih EBV and immunodeficiency
DLBCL associated with chronic inflammation
- forms within sites of longstanding inflammation (e.g., pyothorax)
- EBV+