Nephrotic Syndrome, PIG, IgA, HSP, Pauci, ABGM Flashcards
(63 cards)
Define Segmental
A portion of a glomerulus is involved
Define Global
All of a glomerulus is involved
Define Focal
Some of the glomeruli are involved
Define Diffuse
All or almost all of the glomeruli are involved
-itis
inflammation
-tic
pertaining to
What are podocytes?
Cells of the renal system
What is the four things does the kidney control?
- H20
- RBC production
- acidity
- BP
The kidney filters ______ and passes the _______ to the bladder for _______ as urine.
blood, waste, excretion
What is the average urine physiologic excretion in adults?
80mg/day
Pathologic proteinuria is equal to _____mg or greater over 24 hrs.
150
______ is the smallest plasma protein.
Albumin
- comprises 20-40% of physiologic proteinuria (16-32mg/day)
- Filtered more than other plasma proteins
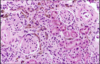
What is this?
Albumin
T/F: microalbuminuria occurs before clinical proteinuria becomes evident and can therefore be used as an early diagnostic tool for early intervention in diabetic patients.
True
Microalbuminuria is defined as excretion of _____ to ______mg/day of albumin
30-300mg/day
Daily excretion of more than 3.5g of protein is called what?
nephrotic range proteinuria
What is the most common cause of proteinuria?
glomerular disease
What is the pathophys of Glomerular disease?
alteration of glomerular permeability –> injury to podocytes (renal cells), basement membrane, capillary endothelium or the mesangium.
Initially there is excess albumin w/eventual progression to larger proteins
What are 3 causes of proteinuria?
- Glomerular Disease MC
- Overflow proteinuria
- Tubular Proteinuria
What is this?
overproduction of smaller proteins overwhelming the reabsorptive ability of proximal tubule.
Overflow proteinuria
What is this?
Tubulointerstitial dz leads to diminshed reabsorptive capacity of the proximal tubule.
Tubular proteinuria
Glomerular Disease is classified into 2 classes. What are these two classes?
NephrITIC vs. NephrOTIC
Primary vs Secondary
Regardless of the classification, both types of Glomerular Dz cause what 3 things?
- glomerular damage
- hypoalbuminemia (low albumin in the blood since you have proteinuria)
- Biopsy = gold standard = definitive diagnosis
What dz?
inflammatory process w/associated immunologic response that leads to renal glomeruli damage.
*allows blood cell passage*
NephrITIC** syndrome**