Neuro: Eye Disorders Flashcards
(60 cards)
1
Q
- Impaired vision that improves with glasses
A
Refractive Error
- Hyperopia
- Myopia
- Astigmatism
- Presbyopia
2
Q
- Eye too short for Refractive Power of Cornea and Lens –> Light focused Behind Retina
A
Hyperopia
3
Q
- Eye too long for Refractive Power of Cornea and Lens –> Light focused in Front of Retina
A
Myopia
4
Q
- Abnormal Curvature of Cornea resulting in Different Refractive Power at Different Axis
A
Astigmatism
5
Q
- Decrease in Focusing Ability during Accomoodation due to Sclerosis and Decreased Elasticity
A
Presbyopia
6
Q
- Inflammation of Anterior Uvea and Iris w/ Hypopyon (sterile pus)
- Accompanied by Conjunctival Redness
- A/w Systemic Inflammatory disorders (e.g. Sarcoid, Rheumatoid arthritis, Juvenile idiopathic arthritis, TB,
HLA-B27-associated conditions)
A
Uveitis
7
Q
- Retinal Edema and Necrosis leading to Scar
- Often viral; CMV, HSV, HZV
- A/w Immunosuppression
A
Retinitis
8
Q
- Acute, Painless monocular vision loss
- Retina cloudy w/ attenuated vessels and “Cherry-red” spot at the fovea
A
Central Retinal Artery Occlusion
9
Q
- Blockage of Central or Branch retinal vein due to compression from nearby arterial Atherosclerosis
- Retinal hemorrhage and edema in affected area
A
Retinal Vein Occlusion
10
Q
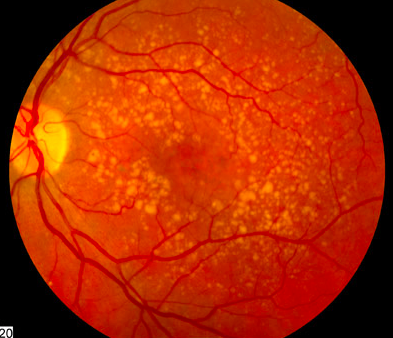
- Retinal damage due to Chronic Hyperglycemia
- Formation of Capillary microaneurysms
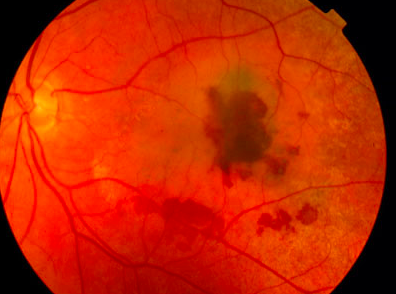
- Hemorrhages, Arteriolar Hyalinization, Cotton-wool spots, Neovascularization, and Fibroplasia
- (2) Types:
- Non-proliferative - damaged capillaries leak blood –> Lipids and Fluid seep into Retina –> Hemorrhages and Macular edema
- Tx: Blood sugar control, Macular laser
- Proliferative - Chronic hypoxia results in New blood vessel formation w/ resultant traction on Retina
- Tx: Peripheral retinal photocoagulation, anti-VEGF injections
A
Diabetic Retinopathy
11
Q
A
Uveitis
12
Q
A
CMV Retinitis
13
Q
A
Central Retinal Artery Occlusion
14
Q
A
Non-proliferative Diabetic Retinopathy
15
Q
A
Proliferative Diabetic Retinopathy
16
Q
A
Retinal Vein Occlusion
17
Q
- Optic disc atrophy w/ characteristic Cupping
- Deepening of the Optic Cup –> decreasing Vision
- Increased frequency of Headaches
- Usually w/ Increased Intraocular Pressure (IOP) and Progressive Peripheral Visual field loss
- (2) Classifications of Glaucoma
- Open Angle
- Primary and Secondary
-
Acute (Closed) Angle
- Primary and Secondary
- Open Angle
A
Glaucoma
18
Q
A
Glaucoma
19
Q
- A/w increase in Age, African-American race, Family History, Painless, more common in U.S.
- Primary - Cause unclear, a/w GLC1A gene on Chromosome 1
- Secondary - Blocked trabecular meshwork from WBCs (e.g., uvetis), RBCs (e.g. vitreous hemorrhage), Retinal elements (e.g. Retinal detachment)
A
Open Angle Glaucoma
20
Q
- Primary - enlargement or forward movement of lens against Central Iris (pupil margin) leads to obstruction of normal aqueous flow through Pupil –> Fluid builds up behind Iris –> Pushing peripheral Iris against Cornea and impeding flow through Trabecular meshwork
- Secondary - Hyposcia from Retinal disease (e.g. Diabetes, Vein occlusion) induces Vasoproliferation in Iris that contracts angle
- Chronic closure - Often asymptomatic w/ dmg to Optic nerve and Peripheral vision
- Acute closure - True Ophthalmic emergency. Increase IOP pushes Iris forward –> Angle closes abruptly –> Very painful, sudden vision loss, Halos around lights, Rock-hard eye, Frontal headache. DO NOT GIVE Epinephrine because of its Mydriatic effect
A
Acute (Closed) Angle Glaucoma
21
Q
- Painless, often bilateral, opacification of Lens
- Decrease in vision
- A/w Systemic therapy w/ Glucocorticoids
- A/w Age, Smoking, EtOH, Excessive Sunlight, Prolonged corticosteroid use, Classic galactosemia, Galactokinase deficiency, Diabetes (sorbitol), Trauma, Infection
A
Cataract
22
Q
A
Cataract
23
Q
- Optic disc swelling (usually bilateral) due to Increased Intracranial pressure (e.g. 2nd to mass effect)
- Enlarged blind spot and elevated Optic disc w/ blurred margins seen on Fundoscopic exam
- A/ increased Intra-cranial pressure is NOT Typically a/w Visual loss
A
Papilledema
24
Q
A
Papilledema
25
* Degeneration of Macula (Cental area of Retina)
* Causes Distortion (metamorphopsia) and eventual loss of Central Vision (Scotomas)
* Dry (nonexudative, \> 80%) - deposition of Yellowish extracellular material in and beneath Bruch membrane and Retinal pigment epithelium ("Drusen") w/ gradual Decrease in vision. Prevent progression w/ multivitamin and antioxidant supplements
* Wet (exudative, 10 - 13%) - rapid loss of vision due to bleeding, 2nd to **Choroidal neovascularization --\>** local production of VEGF
* Tx: anti-vascular endothelial growth factor injections (**anti-VEGF**) or laser.
Age-related Macular Degeneration
| (ARMD)
26
Dry Age-related Macular Degeneration
27
Wet Age-related Macular Degeneration
28
* Increase in orbit contents that push the eye forward
* Results in chronic corneal exposure to the air --\> Corneal Ulceration and Infection
* Inferiorly medially: Lacrimal gland inflammation, lymphoma, Pleomorphic adenoma, Adenoid cystic carcinoma
* Axial: Glioma, Meningioma
Proptosis
29
* Proptosis caused by Exracellular matrix (ECM) accumulation and Rectus Muscle fibrosis
* Severity is independent of Thyroid status
Thyroid Ophthalmopathy
| (Graves Disease)
30
* Most common eyelid malignancy
* Predilection for Lower eyelids and Medial Canthus
Basal Cell Carcinoma
31
* Second most common Eyelid malignancy
* Metastisizes first to Parotid and Submandibular lymph nodes
* May form a local mass that mimics Chalazion or may diffusely Thicken the Eyelid
* May resemble inflammatory Blephitis or Ocular Cicatricial Pemphigoid due to intraepithelial spread
* Exhibits Intraepithelial pagetoid spread into the Nasopharynx and Lacrimal glands
* 22% Mortality rate
Sebaceous Carcinoma
32
* Third most common Lesion
* Melanomas are rare
* Tend to follow an indolent course
* A/w HPV type 16 and 18
Squamous Cell Carcinoma
33
* Sebaceous drainage blocked by inflammation
Blephatis
34
* Neoplasm, extravasated lipid provokes a Lipogranulomatous response
Chalazion
35
* Nonkeratinizing stratified squamous epithelium
* Responds to inflammation by forming minute Papillary folds
Palpebral Conjunctiva
36
* Pseudostratified columnar epithelium rich in Goblet cells
* A/w Lacrimal and Lympoid tissues and can be expanded in Viral conjunjuntivitis or Lympoid malignancy
Fornix Conjunctiva
37
* Nonkeratinizing stratified squamous epithelium that covers the surface of the eye
Bulbar Conjunctiva
38
* Common and typically benign
* Rarely involve the Cornea, Fornix, or Palpebral conjunctiva (pigmented lesions)
* Chornic inflammation can occur during adolescence (inflamed juvenile nevus) and involve Lymphocytes, Plasma cells, and Eosinophils
* Contain subepithelial cysts lined w/ surface epithelia
Conjunctival Nevi
39
* Unilateral
* Middle-aged, Fair-complexioned patients
* Have a Intraepithelial phase --\> Primary acquired Melanosis w/ atypica --\> spread through the lymphatics to Regional lymph nodes
* Parotid and Submandibular lymph nodes are favored for Initial Metastatic sites
* 25% Mortality rate
Conjunctival Melanomas
40
* Calcific band keratopathy, a common complication of chronic uveitis
* Calcium deposition in Bowman's layer
* Actinic band keratopathy involves ultraviolet-induced corneal collagen degeneration
Band Keratopathies
41
* Corneal thinning and Ectasia cause the Cornea to become Conical (rather than spherical)
* Distored vision
* Bowman's layer fractures are Hallmarks
* Mtalloproteinase activation may be causal but Inflammation is absent
Keratoconus
42
* Primary loss of Corneal endothelial cells --\> Stromal edema and Bullous Keratopathy (epithelial detachment from Bowman's layer, forming bullae)
* Blurring and loss of Vision
Fuchs Endothelial Dystrophy
43
* Deposits of various stromal proteins (resulting from mutations that affect folding) and form discrete opacities in the Cornea
* Compromising vision
* Deposits adjacent to Epithelium or Bowman's layer can also cause Painful Erosions and Scarring
Stromal Dystrophies
44
* Most common form of Glaucoma
* Intraocular pressures are elevated despite an Open angle and Normal-appearing structures
* Some functional increases in Resistance to Aqueous Humor outflow
* Familial MYOC mutations encoding for the protein Myocilin
* Physical clogging of the Trabecular meshwork, Particulate matter (senescent erythrocytes after trauma, or iris pigment epithelial granules, etc.)
Open-angle Glaucoma
45
* The Peripheral zone of the Iris (a/ tissue) adheres to the Trabecular Meshwork and Physically impedes the Aqueous Outflow from the eye
* May occur as a Primary angle-closure Glaucoma in eyes w/ shallow anterior chambers (pts. are often Hyperopic) or can occur subsequent to Neovascular membrane formation (after trauma) or Ciliary Body tumors
Angle-closure Glaucoma
46
* Non-infectious Uveitis limited to the Eye
* A/w Penetrating eye injury, developing w/in 2 weeks (to many years) after the insult
* Retinal antigens establish a delayed Hypersensitivity response that affects not only the injured eye but also the Contralateral, Uninjured eye
* Bilateral granulomatous inflammation affecting ALL Uveal Components
Sympathetic Ophthalmia
47
* A/w Full-thickness retinal defect developing when Structural collapse of the Vitreous exerts traction on the Retinal Internal limiting membrane
* Liquefied viteous humor then seeps through the tear and separates the neurosensory Retina and RPE
Rhegmatogenous Retinal Detachment
48
* Exudates accumulate or Fluid leaks from the Choroidal circulation beneath the retina (e.g. w/ Choroidal tumors or malignant HTN)
Non-rhegmatogenous Retinal Detachment
| (w/out a Retinal break)
49
* HTN --\> Retinal arteriosclerosis w/ Wall thickening
* Malignant HTN --\> damaged Choroidal vessles can cause Choroidal Infarcts (?) or Exudate accumulation between the Neurosensory retina and RPE --\> detachment
Elschnig Pearls
50
* Immature Retinal vessels respond to increased Oxygen tension (administered to premature infants) by constricting --\> resulting in local Ischemia
Retinopathy of Prematurity
| (Retrolental Fibroplasia)
51
* Collection of fairly common inherited disorders that affect various aspects of Vision
* Including Visual cascade and cycle, Structural genes, Transcription factors, Catabolic pathways, and Mitochondrial metabolism
* Night blindness caused by loss of rod photoreceptors is an early symptom --\> Eventual loss of Cones too
* Branching reticulated pattern to the Retina
* Optic disc may appear pale and waxy pallor
* Attenuation of Retinal blood vessels
* Both Rods and Cones are lost to Apoptosis and there is a/ Retinal Atrophy w/ Perivascular Retinal Pigment Accumulationkl;
Retinitis Pigmentosa
52
* Blood supply to the Optic nerve can be interrupted by Vascular inflammation (e.g. Temporal arteritis) or by Embolism or Thrombosis
Anterior Ischemic Optic Neuropathy
53
![]()
Tay-Sachs Disease
"Cherry-red Spot"
54
* Pupillary Light-near Dissociation
* No Direct or Consensual Light reflex
* Accommodation - Convergence Intact
* A/w **Neurosyphilis**, Diabetes
Argyll Robertson Pupil
55
* Lesion of Afferent Limb of Pupillary light reflex
* Diagnosis made w/ swinging flashlight
* Shine light in affected pupil --\> pupils do not constrict fully
* Shine light in normal eye --\> pupils constrict fully
* Shine light immediately again in affected eye --\> apparent dilation of both eyes because of stimulus carried through that CN II is weaker
* A/w Multiple Sclerosis
Marcus Gunn Pupil
| (Relative afferent)
56
* Caused by a lesion of the Oculosympathetic Pathway
* Syndrome consists of Miosis, Pthosis, Apparent Enophthalmos, and Hemianhidrosis
Horner Syndrome
57
* Dilated pupil that reacts sluggishly to light, but better to Accommodation
* Seen in Women and a/w Loss of Knee Jerks
* Ciliary ganglion lesion
Adie Pupil
58
* Increased Intraocular pressure --\> Leads to Uncal herniation --\> CN III Compression --\> Fixed and Dilated Pupil
* "Down-and-Out" eye, ptosis
Uncal Herniation
Transtentorial Herniation
59
* Most common cause of Corneal ulcers
* Intranuclear inclusions
* Perforate through the globe --\> medical emergency
* Chornic herpetic corneal infections --\> Localized Opacity
* Lymphocytes, Plasma cells, Viral inclusions in Corneal Epithelial cells are present
Herpes Simplex Virus
60
* Most common malignant ocular neoplasm in children
* Clusters of Cuboidal or Short Columnar cells around a Central lumen "Flexner-Winter-Steiner Rosettes"
* Can spread to the Orbit or along the Optic Nerve
Retinoblastoma


