Neurology ABIM Flashcards
(120 cards)
Primary Headaches
- Types (name 3)
- primary headaches make up 90% of headaches
- migraines
- tension
- trigeminal autonomic
Migraine Headache
- Diagnosis (POUND)
Diagnosis:
Migraine is the most common headache in clinical practice
Four or more features are 90% predictive of migraine headache
- Pusatile quality
- One day duration (4-72 hours)
- Unilateral location
- Nausea or vomiting
- Disabling intensity (patient goes to bed)
Migraine Headache
- Aura signs
- Brainstem aura signs
- Aura complex with some degree of motor weakness
30% of patients with migraines experience aura; lasts 5-60 minutes
- Aura: visual loss, hallucinations, flashing lights, numbness, tingling, aphasia, confusion
- Brainstem aura: vertigo, ataxia, dysarthria, diplopia, tinnitus, hyperacusis, or alteration in conciousness
- Hemiplegic migraine: any aura + some degree of motor weakness
Tension Headache
- Time frame
- Unilateral or Bilateral
- Quality
- Effect on activity
- Nausea?
- Treatment (acute)
- Prophylaxis
Tension Headache
- Time frame: 30 mins - 7 days
- Unilateral or Bilateral: Bilateral
- Quality: Pressure or tight
- Effect on activity: Does not prohibit
- Nausea? No
- Treatment: NSAIDS
- Prophylaxis: TCAs (amitriptyline)
Trigeminal Neuralgia:
- Quality
- Distribution
- Triggered by
- Testing
- Treatment
Trigeminal Neuralgia:
- Quality: Brief paroxysms
- Distribution: Unilateral, stabbing, piercing; V2-V3 distribution of trigeminal N.
- Triggered by: light touch of affected areas
- Testing: Obtain an MRI to exclude intracranial lesions
- Treatment: Carbamazepine i.e. tegretol (anticonvulsant that works by decreasign nerve impulses that cause seizures and pain)
Medication Overuse Headache
- Quality
- Duration
- Medications
- Treatment
Quality/Duration/Meds:
- Chronic headache > or = to 10 days per month using combination analgesics, ergotmaine products, triptans
- Chronic headache > 15 days per month in patients using simple analgesics
Treatment:
- Must withdrawal all pain medications
Chronic Migraine Headache
- Duration (days/months)
- Features
- Risk factors
Duration
- Headache occuring > or = 15 days for > 3 months
Features
- Features of migraine > or + to 8 days per month
Risk Factors
- mirgraine headache frequency or acute medication use > 10 days per month
Migraine: Treatment - Acute
(categorized as: acute, prophylactic, rescue)
- Acute
- mild-moderate
- severe, not relieved
- present on awakening
- migraine-associated nausea
Acute:
- mild-mod: aspirin, NSAIDs
- severe: triptan or dihydroergotamine
- present on awakening or w/vomiting: nasal or subcutaneous sumatriptan
- nausea: metoclopramide, prochlorperazine
Migraine: Treatment - prophylactic
(categorized as: acute, prophylactic, rescue)
- Evidence-based migraine prophylaxis (non pregnant patients)
- amitryptiline (TCA)
- metoprolol
- propranolol
- timolol
- topiramate
- valproic acid
- venlafaxine
What is the treatment for a chronic migraine?
Onabotulinum toxin A
Migraine Tx Contraindications
- What must be avoided in women experiencing aura with migraine and why?
- Which migraine medication is contraindicated in CAD, cerebrovascular disease, brainstem aura and hemiplegic migraine?
- Estrogen-containing contraceptives
- Triptans (due to vasoconstriction)
Migraine Prophylaxis
- In what 4 scenarios do you choose migraine prophylaxis?
- migraines do not respond to therapy
- headache occurs > or = 10 days per month
- disabling headache occurs > or equal to 4 days per month
- use of acute migraine medications is > 8 days per month
Trigeminal Autonomic Cephalgias
- Name the 4 types
- characterized by:
- severity?
- unilateral or bilateral?
- location?
- accompanied by?
4 types:
- Cluter, Chronic paroxysmal hemicranias, SUNCT, Hemicrania Continua
Characterized by:
- Quality: severe
- Unilateral pain
- 1st division of trigeminal N (periorbital, frontal, temporal)
- accompanied by ipsilateral autonomic symptoms
Trigeminal Autonomic Cephalgias
Pain, Duration, Treatment
- Cluster
- Chronic Paroxysmal Hemicranias
- SUNCT
- Hemicrania Continua
Cluster: perioorbital, 15-180 mins, several x per day. repeats over weeks. dissaperas for months or years. unilateral tearing, rhinorrhea, eyelid edema, miosis, ptosis. Acute: triptan or O2; Long term prevention: Verapamil
CPH: At least 5x/day. Lasts 2-30 mins. Indomethicin.
SUNCT: Dozens to hundreds x per day, 1-600 seconds. Resistant to treatment.
HC: Persistent unilateral headache that responds to indomethicin.
Secondary Headaches
- Signs and Symptoms (usually display “red flags”)
- first or worst headache
- abrupt osnet or thunderclap attack
- progression or fundamental change in headache pattern
- abnormal physical examination findings
- neurologic symptoms lasting > 1 hour
- new headache in persons > 50 years old
- new headache in patients with cancer, immunosuppression, pregnancy
- association with alteration in or loss of conscoioussness
- headache triggered by exertion, sexual activity, valsava maneuver
Secondary Headaches:
- What tests to order? (as appropriate)
- MRI over CT in nonemergent situations
- CT for suspected acute ICH
- ESR or CRP for Giant Cell Arteritis
- LP for suspected infectious or neoplastic meningitis or disorders of intracranial pressures
*EEG has no role in assessment of headache disorders
Thunderclap Headaches
- Definition:
- Name 4 important thunderclap headaches
Defined: reaching maximum intensity within 1 hour
- Subarachnoid hemorrhage
- Carotid or Verterbral Dissection
- Thrombosis of cerebral vein or dural sinus
- Reversible cerebral vasoconstriction syndrome
Subarachnoid Hemorrhage
- Clues
- Treatment
Clues:
- Sudden onset of “worst headache of my life”
- Warning “sentinel” headaches (leakage of blood from brain headache)
Treatment:
- Neurosurgery in selected cases (85% of nontraumatic cases caused by ruptured aneurysm)
Carotid or Vertebral dissection
- Clues
- Treatment
Clues
- Neck pain and ipsilateral headache
- Neurologic findings in territory of vessel involved
Treatment
- Aspirin, heparin, or oral anticoagulation (dissection exposes tissue factor in artery wall, these medications prevent thrombotic event, stroke)
Thrombosis of Cerebral Vein or Dural Sinus
- Clues
- Situations to consider
- Treatment
Clues
- Exertional headache
- Papilledema
- Neurologic findings
Situations
- Consider in hypercoaguable states, pregnancy, use of OCPs
Treatment
- LMWH followed by warfarin
Reversible Cerebral Vasoconstriction Syndrome
- Clues
- Associated with
- Imaging
- Treatment
Clues: Recurrent thunderclap headache syndrome, more frequent in women
Associated with:
- Pregnancy, neurosurgical procedures, exposures to androgenic or serotenergic drugs
Imaging:
- strokes, hemorrhages, or cerebral edema
Treatment: Normalization of BP, elminate triggering drug/substance, glucocorticoids may worsen outcomes
Idiopathic Intracranial Hypertension
(pseudotumor cerebri)
- Definition
- Typical patients
- What is nearly always present?
- Confirm diagnosis
- Imaging findings
- First-line treatment
Defined: increased intracranial pressure w/o identifiable structural pathology
Typically: Female, obese, child-bearing age
Nearly always present: Papilledema
Confirmation: CSF pressure > 250 with normal fluid composition
Imaging: MRI may be normal or show small ventricles, widened optic nerve sheeths or partially empty sella
First-line Treatment: Acetazolamide (Diamox; CA inhibitor; reduces edema, reduces pressure)
Traumatic Brain Injury
- Presentation
- mild
- postconsussion syndrome
- hematomas
- rapid neurologic decline
mild TBI: LOC, “dazed” after head injury, amnesia near the time of event, FN deficit
postconcussive sydrome: persistence of symptoms of mild TBI beyond typical recovery period of several weeks
hematomas: may result in epidural or subdural hematomas presenting with headache and mental status abnormalities
rapid neurologic decline: may occur; with ipsilateral pupillary dilatation and brain herniation
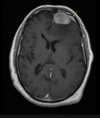
Epidural Hematoma
- Signs
- CT scan
Signs:
- headache
- mental status abnormalities
- loss of consiousness with brief lucid interval before subsequent decline
CT scan:
- bioconvex lens between skull and out margin (dura)