Neuromuscular Junction (Ferguson) Flashcards
(23 cards)
Neuromuscular diseases are conditions that involve pathology in the _______, ________, ________, ________, _______ and/or ______ in the brainstem or spinal cord
- Muscle
- Neuromuscular junction
- Peripheral nerves (including CN)
- Spinal nerve roots
- Nerve plexus
- Motor nerve nuclei
Normal anatomy and physiology of the neuromuscular junction;
- releases more ACh than needed for muscle movement - becomes saturated

What diagnosis?
- Bimodal distribution - what ages?
- Presentation can be generalized, bulbar (CN), or ocular
- Symptoms are worse at the end of the day
Myasthenia Gravis
- Teens - 30 (females); 50-70 (males)
What changes can you see on EM?

Due to chronic inflammation - see decreased surface area, decreased # of receptors, leading to the propensity to be much weaker!
Pathophysiology of Myasthenia Gravis:
- Blocking of the skeletal muscle _____ ____ site!
- Accelerated ______ and ______ of AChr caused by crosslinking by the IgG antibodies
- _______ - mediated lysis of the muscle end plate. This results in distortion and simplification of the muscle end plate
- Nicotinic ACh receptor
- internalization, degradation
- Complement
- What is the role of the thymus in MG?
- thymocytes in culture spontaneously produce anti-AChR ab
- In ACh-receptor antibody positive MG patients - 50% have ______, 10-15% have a ______
- Remains unclear - but it houses all the functional components to produce the immune response seen in MG
- May be involved in initiation and maintenance
- 50% thymic hyperplasia
- 10-15% thymic tumor

MG has a highly variable symptomatology!!!
- Often there is a history of fluctuating weakness of extraocular, oropharyngeal, axial, limb muscles
- 2 pearls?
Fatiguing Maneuvers?
- Can you name some?
- “fatigable weakness” diurnal variation”
- Sustained upgaze (30-60 sec) [medial rectus most likely involved]
- Sustained abduction of arms (120 sec)
- Sustained elevation of leg while laying supine (90 sec)
- Repeated rising from chair without arm use (up to 20 sec)
- Counting out loud (watch breaths 1-50) [dysarthria, sob may be enhanced]
What is:
- the most common antibody in MG
- Found in 80-85% of myasthenics
- only presents in 50% of isolated ocular cases
- Low false positive number (solid specificity)
- “GOLD STANDARD” lab analysis
Anti-ACh receptor antibody
What is:
- NMJ protein that plays a role in clustering ACh receptors
- Typically seen in generalized MG
- rarely seen in isolater ocular MG
- presents in up to 40% of ACh receptor binding antibody negative patients
Anti-muscle specific tyrosine kinase
What is:
- First antibody discovered in MG
- Very highly associated with thymoma
- Present in 75-80% of those with the tumor
- also present in non-tumor settings
- Study is utilized most often in 2 settings:
- Young, newly diagnosed patients as adjunct to help detect thymoma
- Older patients with mild disease, where this could be the only abnormality
Anti-striated muscle antibody
What electrodiagnostic test:
- The sensitivity for diagnosing MG ranges from 53% to 100% in generalized MG, and 10-17% for ocular MG
- If this test is normal and a high suscpicion for an NMJ disorder exists, SFEMG of at least one symptomatic muscle should be performed
Repetitive nerve stimulation
What test:
- ACh-esterase inhibitor that can be administered via IV at bedside
- Advantages: assess for improvement in ptosis, weakness
- Rapid onset: 30 sec
- Short duration of effect: 5-10 min
- Sensitivity: 71-95% for generalized MG
- Drawbacks:
- must blind physician to drug vs placebo
- side effects: bradycardia, hypotension
- not reliable in anti-MuSK MG
- not very specific to the diagnosis of MG
- Advantages: assess for improvement in ptosis, weakness
Edrophonium (Tensilon) Test
Symptomatic treatment for MG:
- A cholinesterase inhibitor
- Increases the size and length of end plate potential
- Onset is within 30-45 minutes with loss of effect between 3-6 hours
- SE: stomach cramps, diarrhea, sweating, increased bronchial and nasal secretions, bradycardia, N/V –> decrease dose to minimize side effects
Pyridostigmine (Mestinon)
What short term immunosuppressant treatment of MG:
- temporarily reduces the levels of circulating ab
- most patients see symptomatic improvement in days
- typical course is 3-6 scheduled every other day
- not every day - DEPLETES CLOTTING FACTORS
- Often used for exacerbations, or employed regularly scheduled basis in multidrug resistant patients
Plasma exchange {PLEX}
What short term immunosuppressant therapy for MG:
- Comparable to PLEX
- Mechanism of action: unclear- neutralizing vs. down regulation
- symptoms improve within days and effects last between 4-8 weeks
- Dosed at 2 g/kg divided over 2-5 days
- Like PLEX, it is used in exacerbations and in resistant cases
IV immunoglobulin
Long term immune-directed therapies for MG:
A: One absolute indication - presence of thymoma; not emergent
- Beneficial for patients younger than 50 years old
B: Short term Drug?
C: Long term Drugs? (for life)
A. Thymectomy
B: Corticosteroids
C. Chemo - azathioprine, mycophenolate
Diagnosis?
- Approximate incidence: rare
- M:F - equal! (previously 70:30)
- Strong association with small cell lung cancer - found at least 3% of SCLC patients
- Slightly more than 1/2 of patients with this have an identifiable malignancy
- Age of onset is typically mid to late adulthood
- Non SCLC is typically found in younger females who have other autoimmune diseases
Lambert Eaton Myasthenic Syndrome
What is the pathophysiology of Lambert eaton syndrome?
- AB made in response to an antigen that SCLC expresses
- Cross links multiple channels - making them ineffective by disrupting their proper positioning and function
Decreased influx of _____ leads to decreased ____
- Less binding to receptors - decreased _______
- Can result in failed transmission and low CMAP
IgG ab binding to voltage gated Ca channels in the presynaptic neuron
Calcium, acetylcholine
- end plate potential
Presentation of Lambert eaton:
- No history of ____ necessary
- Slowly progressive _______ weakness (ache or tenderness)
- ____ and _____ symptoms typically very mild
- Taste?
- Will have weakness when on what type of medication?
- Prolonged paralysis following paralytic drug given prior to intubation
- cancer
- proximal leg or arm
- bulbar, respiratory
- Dry mouth, metallic taste
- Calcium channel blockers
Approximately 3% of all SCLC patients have ____
- May precede diagnosis by 9 months - up to 2 years, but rare
- Smoking history and age > 50 are strong indicators that there is cancer present
PE:
- Proximal weakness with improves with exercise
- Minimal bulbar findings - occasionally, ptosis, blurred vision, difficulty chewing, dysphagia, dysarthria
- Dry eyes, dry mouth frequently reported
- Reduced/absent DTR’s; normal sensory exam
Lambert Eaton Myasthenic syndrome
How is LEMS diagnosed?
- look for VGCC antibody
- repetitive stimulation: 3 hz, 30-50 hz.

- Serum testing
- Electrodiagnostic testing
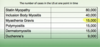
FYI: see chart
Treatment for LEMS - symptomatic and immunosuppressive treatments similar to MG, just less effective
- No role for thymectomy, need emergent tx with PLEX and IVIg