Neuropsych Flashcards
(32 cards)
Depression Pathophysiology
- All antidepressants effect monoamine system and neurotransmitters (NT)
- Serotonin (5-HT), norepinephrine (NE), and/or dopamine (DA)
-
Monoamine Hypothesis: Decrease in function or amount of NT in the brain
- Treatment increases NT immediately, but effects on symptoms are delayed
-
Neurotrophic Hypothesis: Adaptive Changes to Amine Receptor Systems
- Desensitization or downregulation of receptors
- Disrupted Brain-Derived Neurotrophic Factor (BDNF)
- Growth factor protein that regulates differentiation & survival of neurons
Antidepressant Classes
- Selective Serotonin Reuptake Inhibitors (SSRI)
- Fluoxetine has the most evidence to support its use in the adolescent population
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRI)
- Tetracyclic and Unicyclic Antidepressants
- Not Recommended in children:
- Tricyclic Antidepressants (TCA)
- Monoamine Oxidase Inhibitors (MAOI)
Receptors and Transporters
- ACh M: acetylcholine muscarinic receptor
- Anticholinergic effects (dry)
- H1: histamine1 receptor
- Sedation, HOTN, weight gain
- 5-HT2: serotonin 5-HT2 receptor
- Sedation, HOTN, sexual dysfunction
- Bleeding risk – impairment of platelet aggregation with serotonic-affecting agents
- NET: norepinephrine transporter
- NE reuptake inhibition: decreased depression, tremors, tachycardia, sexual dysfunction
- SERT: serotonin transporter
- Serotonin reuptake inhibition: decreased depression, anxiety, GI distress, sexual dysfunction
Affinity
- • 0/+, minimal affinity +, mild affinity
- • ++, moderate affinity +++, high affinity
SSRI
- MOA - Inhibition of serotonin transporter (SERT)
- Many Treatment Indications - broad spectrum of use
- First line treatment option
- Safe in overdose
- Relative tolerability
- Consider variability within class
- Consider Drug Interactions
- Enhance serotonergic activity
- GI – n/v/d/GI issues (start early and improve with time)
- Diminished sexual function and interest
- 30-40% loss of libido, delayed orgasm, diminished arousal
- Headaches
- Insomnia, hypersomnia
- Excessive sleepiness or trouble staying awake during the day; can fall asleep at any time
- Weight gain (especially paroxetine)
- “Disinhibition” (risk-taking behaviors, increased impulsivity)
- Increase risk of bleeding
- Citalopram/Escitalopram – prolong QT interval
- SIADH and hyponatremia (Age, volume depletion, diuretic use)
- Prozac t1/2 48-72h; active metabolites t1/2 180 hours – longest
- Paxil t1/2 20-23h – shortest

Serotonin-Norepinephrine Reuptake Inhibitors (SNRI)
- Similar serotonergic effects to SSRIs
- Increased risk of bleeding
- Noradrenergic effects: Dose-related hypertension; tachycardia
- CNS activation: insomnia, anxiety, agitation
- Increased sweating and urinary retention
- SIADH and hyponatremia (Risk factors - volume depletion, diuretic use)
- Increase risk of seizures
-
Duloxetine
- Hepatotoxicity; Hyperglycemia
-
Venlafaxine
- Dyslipidemia (Total cholesterol, TG)

Tetracyclic and unicyclic
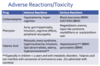
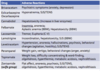
Tetracyclic & Unicyclic Adverse Reactions
-
Bupropion
- Improves sexual dysfunction; not sedating; no weight gain
- Agitation, insomnia, anorexia; hypertension
- Seizure risk especially in overdose
- Contraindicated in patients with seizure disorders & eating disorders
-
Mirtazapine
- Sedative effect; weight gain; sexual dysfunction
- Anticholinergic effects (dry mouth, constipation, orthostatic hypotension)
- Increased arrhythmias (QT prolongation, V Fib)
- Hyperlipidemia; hyponatremia

Serotonin Syndrome
-
Overstimulation of 5-HT receptors
- Serotonin antidepressant + other serotonin medications
- (Linezolid; dextromethorphan, sumatriptan, tramadol, methadone, St. John’s wort)
- Triad of Symptoms
- Cognitive (delirium, coma) +
- Autonomic (hypertension, tachycardia, diaphoresis) +
- Somatic (myoclonus, hyperreflexia, tremor)
- Caution when switching from one serotonin antidepressant to another, especially Fluoxetine with longer t 1⁄2; allow 1-2 weeks washout period
Antidepressant Discontinuation Syndrome/Withdrawal Syndrome
- Avoid abrupt discontinuation of antidepressant therapy
- Taper dose over several weeks with consideration to half-life
- Reduce dose every 5-7 days
- Longer duration for medications with shorter t1⁄2 • Fluoxetine taper may be unnecessary
- Long term therapy - taper over 4-6 months
- If symptoms occur during taper, restart at the original dose taper slower
- Especially if short half-lives; case reports with all drugs
- Differentiate from relapse of depression or other psychiatric/medical conditions
-
F.I.N.I.S.H. Mnemonic for recognition of symptoms
- Flu-like symptoms (general malaise, muscle ache, headaches)
- Insomnia
- Nausea - GI disturbances
- Imbalance - Dizziness/lightheadedness, vertigo
- Sensory disturbances - paresthesia, visual disturbance
- Hyperarousal - anxiety, agitation
- Symptoms resolve within 1-2 weeks; Not life-threatening
AAP Recommendations – Selecting Therapy
First Line – SSRI
- Base selection on optimum combination of safety and efficacy data including drug interactions
- Deliberate self-harm and/or suicide risk is more likely if SSRI started at higher doses
- Only fluoxetine FDA approval ≥6yo for depression
- Also approved for depressive episodes associated with bipolar I disorder (in combo w/ olanzapine ≥ 10yo); and OCD ages ≥7yo
- Escitalopram only FDA approved >12yo for depression
- *Sertraline FDA approved ≥ 6yo for OCD
- Details regarding initial selection of specific SSRI and possible reasons for initial drug choice in GLAD-PC toolkit
Selecting between SSRIs
- FDA approval for adolescents
- If no contraindications, fluoxetine recommended as first-choice • Success of prior medication trials
- SSRI half-life
- Interactions with other medications
- Side effect profiles of different medications
- Family history of successful medication treatment
- Patient’s medical issues
AAP Recommendations – During Treatment
- Delayed improvements in symptoms
- Consider titrating dose after 2-3 weeks if no positive response noticed
- Reassess diagnosis/ initial treatment if no improvement noted after 6 to 8 weeks and consider mental health consultation
- < 50% of patients respond to 1st line therapy
- Maintain therapy for 6 to 12 months after full resolution of depressive symptoms
- Regardless of length of treatment, monitor all patients on a monthly basis for 6 to 12 months after full resolution of symptoms
- If patient experiences a recurrence, clinicians are encouraged to monitor patients for up to 2 years given high rates of recurrence
- Switch within a class before switching to another class

ADHD
- Eval for ADHD for any child 4-18yo presenting with academic or behavioral problems and symptoms of inattention, hyperactivity, or impulsivity
- Pre-school: EBP behavior therapy first; methylphenidate if not improved
- Elementary: drug and/or behavior therapy, preferably both
- Evidence stronger for stimulant medications and sufficient but less strong for atomoxetine, extended release guanfacine, and extended release clonidine (in that order)
- Adolescent: drug and/or behavior therapy, preferably both
- ER formulations more expensive, but benefits of consistent & sustained coverage with fewer administrations, better adherence
- Some adolescents, might require > 12 hours of coverage: utilize a short-acting might be used in addition to long-acting
- Identify risk factors for Stimulant Medications
- History of cardiac symptoms; cardiac family history (arrhythmias, sudden death, death at young age from cardiac conditions); vital signs, cardiac physical examination
- Presence of tic disorder: affects ~20% of patients with ADHD
- Stimulant medication does not clearly worsen tics, may do so in individual cases. Atomoxetine or alpha-agonist may lessen comorbid tics.
- Minimization of adverse effects
- Affect on sleep initiation
- Risk status for drug use/abuse
AAP Recommendations – Initiating ADHD Therapy
- Begin with low dose and titrate to dose that provides maximum benefit and minimal adverse effects
- During 1st mo of trx, titrate weekly/biweekly via discussions w parents
- Stimulant medications can be effectively titrated on a 3 to 7 day basis
- In-person follow up recommended by 4th week of therapy
- Initially, core symptom reduction is more likely to indicate medication effects
- Effects of improvement in function require more extended time period
- If max dose reached without satisfactory results or intolerable effects, switch to another stimulant before attempting non-stimulant
Stimulant Medications
Methylphenidate or amphetamine compounds
- MOA: Affect CNS dopaminergic pathways
- First choice of treatment
- > 70% of children and youth with ADHD respond to 1st stimulants at an optimal dose; 90-95% respond to 2nd stimulant
- Highly effective for most children in reducing core sx of ADHD
-
ADME Consideration:
- Children 4-5 years of age have slower rates of metabolizing methylphenidate, initiate a lower dose and increase in smaller increments
- AE: generally dose dependent
- Most Common AE
- Appetite loss, abdominal pain, headaches, and sleep disturbances
- Decreases growth velocity (~1-2 cm)
- Esp in higher, consistently administered doses
- Effects decrease by 3rd year of trx
- Uncommon: hallucinations and or psychotic symptoms
- Rare occurrence of sudden cardiac death; depression, suicidal ideation
- AE in preschool-age children – increased mood lability and dysphoria
Non-stimulant Medications for ADHD
- First choice of treatment if concerns about possible abuse/diversion or strong family preference against stimulant medication
- Take longer to reach efficacy
Atomoxetine
- May also be effective for comorbid mood or anxiety disorders and has no abuse risk
Guanfacine and Clonidine
- Also beneficial as alternatives or adjuncts to stimulant treatment
- Useful in combination with stimulants for comorbid sleep problems, tics, or Tourette syndrome
- Potential advantages of guanfacine over clonidine include fewer sedative and hypotensive effects
Atomoxetine
- MOA: Selective norepinephrine-reuptake inhibitor
- Maximum response may take ~4 to 6 weeks
-
BB Warning on possibility of suicidal ideation when initiating medication management
- Early symptoms of suicidal ideation might include thinking about self harm and increasing agitation
- AE
- Initially - GI symptoms and sedation (initiated at 50% of dose in 1st week)
- Appetite suppression
- Rare: hepatitis
Guanfacine and Clonidine
- Available: Extended-release guanfacine; extended-release clonidine
- MOA: Selective α2A-adrenergic agonists
- Maximum response may take ~2-4 week
- Qday or BID
-
AE
- Somnolence and dry mouth
- Taper when discontinue to prevent rebound hypertension
Epilepsy: Initiating Antiepileptic Therapy
- Will always involve neurology
- Considers
- Seizure type
- Adverse Reaction profile
- Drug interactions and Comorbidities
- Cost and ease of use; patient factors
- Initiate single agent; titrate to efficacy or intolerable SE
- Switch to another agent; titrate to efficacy or intolerable SE
- Attempt dual therapy if monotherapy not effective
- Withdrawal of therapy
- Do not discontinue abruptly
- Gradually taper dose down
Non-epilepsy indications:
- Mood disorders
- Refractory pain syndromes
- Trigeminal neuralgia
- Migraine headaches
- Drug withdrawal syndromes
- Social phobias
First Generation – Older Agents
- Phenobarbital
- Phenytoin (Dilantin®)
- Carbamazepine
- Oral – Carbatrol®, Tegretol®)
- New IV - Carnexiv®
- Valproic Acid
- Valproic Acid (Depakene®)
- Valproate (Depacon®)
- Divalproex (Depakote®)
- Absence Seizures
- Ethosuximide (Zarontin®)
- Adjunctive Therapy
- Acetazolamide (Diamox®)
Second Generation – Newer Agents
- Felbamate (Felbatol®)
- Lamotrigine (Lamictal®)
- Topiramate (Topamax®)
- Levetiracetam (Keppra®)
- Oxcarbazepine (Trileptal®)
- Zonisamide (Zonegran®)
- Lacosamide (Vimpat®)
- Rufinamide (Banzel®)
- Vigabatrin (Sabril®)*REMS
- Ezogabine (Potiga®)
- Perampanel (Fycompa®)
- Brivaracetam (Briviact®)
- Eslicarbazepine (Apiom®)
Other therapies for Epilepsy
-
Benzodiazepines for Status Epilepticus
- Diazepam; Midazolam; Lorazepam
-
Benzodiazepines for Adjunctive Therapy
- Clonazepam (Klonopin®)
- Clorazepate (Tranxene®)
- Clobazam (Onfi®) – 2011
- Adjunctive therapy for Lennox-Gastaut Syndrome
-
Cannabinoids
- Cannabidiol (Epidiolex®) - Approved June 2018
- Lennox-Gastaut Syndrome or Dravet Syndrome
- C-V status
- CBDV (GWP42006) in the pipeline – Phase 2
- Cannabidiol (Epidiolex®) - Approved June 2018
MOA of Neurotransmitters
Excitatory Neurotransmitters
- Glutamine
- Glutamate
Inhibitory Neurotransmitters
- GABA
- Glycine
Goal: Limit sustained repetitive firing & Increase Inhibitory; Decrease Excitatory
- Stabilization of cell membrane
- Prevention of further depolarization
- Decrease impulse transmission
- Increase seizure threshold
-
Targets at Inhibitory, GABAergic Synapse
- GOAL: Increase GABA concentrations
- Enhance synaptic release
- Increase GABA receptor activation
- Block GABA reuptake
- Inhibit GABA transaminase mediated metabolism
- GOAL: Increase GABA concentrations
-
Targets at Excitatory, Glutamatergic Synapses
- GOAL: Decrease circulating glutamate
- Blocking voltage-gated sodium channels **
- Inhibiting voltage-gated calcium channels
- Inhibiting voltage-gated potassium channels
- GOAL: Decrease circulating glutamate
- Sometimes mechanism of action still unclear….

Carbonic Anhydrase Inhibitors
-
MOA: inhibit membrane-bound and cytoplasmic forms of carbonic anhydrase
- Carbonic anhydrases are enzymes that catalyze the conversion between CO2 and bicarbonate
- Inhibition of specific carbonic anhydrases (CA II, CA VII) exhibit anti-seizure activity
- Prevents replenishment of intracellular bicarbonate and depresses the depolarizing action of bicarbonate through GABAA receptors
- Examples: Acetazolamide, Topiramate, Zonisamide
First Gen - Older Agents
Carbamazepine (Tegretol®)
- PK: Metabolized to carbamazepine-10,11-epoxide
- Active metabolite w/increases in side effect
- Auto-inducer
- Broad-spectrum inducer
- Avoid use in patients carrying HLA-B*1502 allele (Asian descent) (BBW)
- Screened prior to initiating therapy
- Increased risk of developing SJS/TENS
Phenobarbital
- Metabolism
- Substrate of CYP450 2C19
- Broad-spectrum inducer
-
MOA: Binds to GABAA Receptors
- Increase the duration of the GABA-gated channel openings
- Less selective actions
- Increases GABA Activity
- Decreases Glutamic Acid Activity – Binds to AMPA receptor
Phenytoin/Fosphenytoin
-
Phenytoin (Dilantin®)
- IV Phenytoin must be administered slowly (50 mg/min)
- BBW with IV administration:
- Hypotension & severe cardiac arrhythmias (heart block, ventricular tachycardia/fibrillation)
- “Purple glove syndrome” - discoloration w/edema & limb pain
Fosphenytoin (Cerebyx®) – IV Only
- Prodrug: more soluble form of phenytoin w/less infusion related reactions; Administer more rapidly (150 mg PE/min)
- General PK: Highly protein bound to plasma proteins (albumin)
- Broad-spectrum inducer
Valproic Acid and derivatives
- PK: 90% protein bound
- Displaces other drugs from proteins
- Broad-spectrum inhibitor