Parasites 2: Geohelmints (Ascaris, hookworm, whipworm, strongyloidis) Flashcards
(28 cards)
How are nematodes (round worms) classified?
Soil-transmitted (geohelminths):
- These usually depend on a period of development outside the human host
- Associated with poverty, inadequate hygiene and sanitation
- Often asymptomatic
- Most individuals only have a few worms but in those with many worms and chronic infection -> anaemia, retarded growth and neurological sequelae
- Anti-helminthic treatment can easily solve this
- Helminths are realtively similar, however can be divided by:
- Direct mode of transmission
- Can go straight from anus to mouth without development period in soil
- Modified direct mode of transmission
- Period of development in soil
- Penetration of the skin
- Develop in soil, get ready for infiltration of the skin to go back through oesophagus into intestine
- Direct mode of transmission

What is the life cycle of ascaris lumbricoides?
- Adult worms live in the lumen of the SMALL intestine
- The female is 20 – 25cm long, male about 30cm long
- The female produces 200k eggs per day which are passed in the stool
- Once deposited and the conditions are right (moist, warm and shaded soil), the fertile eggs become embryonated and infective, they then develop within a few days or a few weeks
- Once they are swallowed, the larvae hatch and infect the mucosa and are carried via the portal and then systemic circulation to the lungs
- There the arvae mature for 10 to 14 days
- There they break the alveolar walls, ascend the bronchiolar tree, reach the throat and are swallowed
- Once they reach the small intestine, they develop into adult worms
- It takes about 2-3 months form ingestion of the egg to mature adult – they can live for one to two years
- Intensity of disease is related to the worm burden and light infection are often asymptomatic with serious disease starting with >100 worms

What are the clinical features of ascaris?
- GI phase:
- Sometimes lactose intolerance and micronutrient deficiency
- Worms may ball up and cause obstruction -> most severe complication
- Most common in childen below ten years, likely due to narrow lumen and high worm-burden

How do we diagnose ascaris?

What does ascaris look like under the microscope?

How do we treat ascaris infection?

Which organisms cause hookworm infections?
- Two species that we focus on:
- Ancylostoma duodenale
- This one has large teeth
- Neactor americanus
- This one has dorsal and ventral cutting plates
- Ancylostoma duodenale
- Causes hookworm anaemia and disease
- Affects >700 million people globally
- Impairs physical and intellectual development of children and communities
- Found in all tropical and sub-tropical countries

What is the lifecycle of hookworm infections?
- Simple lifecycle:
- Eggs are passed in the stool and then the eggs hatch in or two days depending on whether the conditions are right (moist shaded soil)
- After 4 or 5 days they become filariform larvae
- This is the infectious stage of the hookworm
- They can survive 3 or 4 weeks of this stage
- On contact with the host, the larvae penetrate the skin and then travel through the blood to the heart and then to the lungs
- They break through the alveoli, ascend the bronchial tree to the throat and are swallowed
- In the intestine they attach to the wall causing blood loss
- Longevity: up to several years

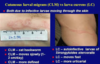
What are the clinical features of hookworm infection?
Most infections are asymptomatic
But gradually worsening anaemia
Initially:
- itch at site of entry with possible pustules and vesiculation
Pneumonitis:
- Dry cough, asthmatic wheezing
- Fever and eosinophilia
- Not common in endemic areas
GI:
- Early:
- Epigastric discomfort
- Late:
- IDA + hypoproteinaemia
*
- IDA + hypoproteinaemia

How do we diagnose a hookworm infection?
Stool exmaination for ova and parasites

How do we treat hookworm infection?

Which organism causes whipworm infection and what is its life cycle?
Trichuris trichiura
- Found in areas with constant sunshine and rainfall
- Few symptoms normally
- But heavy infections can cause GI problems, rectal prolapse, anaemia, growth stunting and cognitive impairment
- Approx. 500 million people infected with whipworm globally in 2010
- Life cycle simple:
- Infective eggs are ingested via contaminated soils or hands
- The eggs are hatched and produce larvae that mature in the colon
- The adult worms of 4cm length live in the caecum and ascending colon
- The worms are fixed in that location but the anterior part go straight into the mucosa
- The females begin laying eggs 60 – 70 days after infection
- Females in the caecum shed up to 20k eggs per day
- The life span is about 1 year
- The unembryonated eggs pass with the stool
- In the soil the eggs develop into a two cell stage, then advanced cleavage and become embryonated
- Become infective in 15 to 30 days

Microscopy of trichuris?

What are the clinical features of trichuris infection?
- Light infection:
- Worms confined to caecum and ascending colon, causing little damage
- Heavy infection
- Worms spred through colon to rectum
- Cause haemorrhages, mucopurulent stools, dysentery, rectal prolapse
- Trichuris dysentery syndrome:
- severe dysentery
- prolapse of rectum
- It’s due to immune response
- Massive infantile trichuriasis
- Children between 3 and 10
- Hypoproteinaemia, severe anaemia, clubbin of fingers
- Growth retardation
- Effect on cognition and later achievements
How do we diagnose trichuris?

How do we treat trichuria?
Mebendazole > Albendazole
Strogyloidiasis facts
Strongyloides stercoralis = threadworm

What is the life cycle of strogyloidiasis?
- Two options
- Free living adult worms that prefer sandy warm moist soil environement
- Straight to infective larvae
- Free living worms:
- Mate and eggs are deposited in soil
- Eggs hatch
- Then develop into adult worms once again
- However, when condition for living become unfavourable, the eggs develop into infective larvae
- Infective larvae can penetrate skin and then usually migrate to lung via blood stream from where they are coughed up and swallowed into GI tract
- Larvae can also migrate directly to GI tract via connective tissues
- Small intestine: larvae multiply and become female adult worms
- There are no adult male worms in the parasitic cycle
- The females live in the wall of the small intestine and produce eggs by parthenogenesis
- The eggs yield rhaptidiform larvae which can be passed in the stool
- In auto-infection the rhaptidiform larvae become infective filariform larvae which can either penetrate the intestinal mucosa or the skin of the perianal area
- In either case, filariform larvae can disseminate through the body
- That is how people develop chronic infections or hyper-infection in immunosuppressed individuals

What are the clinical features of strongyloides infection?

How do we diagnose strogyloides?
- Repeated stool microscopy for rhabditiform larvae
- Hyperinfection: easily diagnosed by exmaining stool, sputum, CSF, etc.
- Duodenal biopsy and miscroscopy of duodenal aspirate
- Detection of filariform larvae
- Flexible gastroduodenoscopy
- String test more practical in resource limited settings
- Serology - for IgG
- Blood count - Elevated WCC and eosinophilia possible
- Generally difficult to diagnose
Microscopy difference strongyloides / ascaris

Microscopy strongyloides filariform larvae

Microscopy duodenal biopsy strongyloides

Treatment strongyloides