Parotid & Temporal Regions Flashcards
(26 cards)
Name the glands indicated in the image from left to right. Which is the largest?

sublingual, submandibular, parotid (largest)
What are the two portions of the parotid gland and what is the nerve that creates this distinction? What surrounds the parotid gland?
Superficial and deep portions separated by the Favial Nerve.
The parotid gland is encompased by parotid fascia
Names the borders of the parotid bed.
- AP: mandibular ramus & mastoid process
- SI: zygomatic arch & mandibular body
- lateral to styloid process
What forms the parotid duct? What is its route?
Formed by tributaries within the parotid gland.
The duct crosses superficial to the masseter, dives into buccal fat & buccinator
Terminates at the 2nd upper molar (parotid papilla)
What is the sensory innervation of the parotid gland?
What is the parasympathetic innervation of the parotid gland?
-
Sensory: auriculotemporal nerve
- branch of mandicular nerve (3rd division trigemina nerve; V3)
- loop around middle meningeal artery
-
Parasympathetic
- from Glossopharyngeal (IX) to otic ganglion to auriculotemporal nerve (from V3) to parotid gland
-
Sympathetic
- from spinal nerve T1-4 to superior cervical ganglion to perivascular plexus on external carotid artery to parotid gland
Name the terminal nerves of Facial Nerve (CNVII) that pass through the Parotid Gland.

“Two Zombie Bit Miley Cyrus”
Temporal
Posterior auricular
Zygomatic
Buccal
Cervical
Marginal mandibular
Name the branches of hte external carotid artery indicated in the image. Which branches supply the parotid gland?

Posterior auricular and branches of maxillary supply parotid gland
Branches from maxillary also support tempromandibular joint and mastication muscles
Name the indicated veins that pass through the parotid gland.
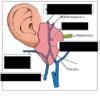
The superficial temporal and maxillary vein combine to produce the retromandibular vein, which will then divide into an anterior and posterior part. The posterior part will merge with the posterior auricular vein to drain into the external jugular vein. The anterior portion will merge with the facial vein.
The blanks from top to bottom
superficial temporal vein
maxillary vein
retromandibular vein
posterior auricular vein
external jugular vein
What lympatic structure is also found in the proximity of the parotid gland? Where do they drain to?
Superficial parotid lymph node– drains part of face and scalp (under eyes to middle of head)
Drains into deep cervical lymph nodes along the internal jugular vein
Parotid tumors are mostly benign and involve the superficial par of the gland. Resection of the tumor could cause damage to which nerve? What would be the implication of this nerve damage?
Facial nerve (CNVII(
loss of innervation to the face
What is the name of the structures that may develop in parotid ducts, causing intense pain while salivating? Are they permanant?
Parotid stones; there are different types of surgeries to remove them
Inflammatin of the parotid gland leads to painful distention (due to fascia). What is the name of this condition and what are its major causes?
Parotitis; due to infection, duct blockages (parotid papilla increases in size)
What is the name of the condition that presents with redness and sweating anterior to ear, specifically associated with eating? What causes this condition?
Frey’s syndrome; caused by parasympathetic nerve damage post-surgery
Name the boundaries of the temporal fossa. What are the contents of the temporal fossa?
Superior temporal line
zygomatic arch
Infratemporal crest of sphenoid
frontal process of the zygomatic bone
zygomatic process of the frontal bone
Contents
- Pterion (landmark- “H” suture line)
- Temopralis muscle
- Nerves :
- deep temporal (2) - innervate temporalis muscle
- Zygomaticotemporal - cutaneous lateral forehead sensation
- Arteries
- deep temporal (2) (from maxillary) - supply temporalis
- middle temporal (from superficial termporal) - anastamoses with deep temporal arteries

What type of joint is the TMJ? What type of cartiladge lines the TMJ join?
synovial; fibrous cartilalidge
Provide the anatomical names for the folowing actions and explain what is occuring at the TMJ for the action to occur.
- closing the mouth
- opening the mouth
- pushing chin backwards
- bringing chin forwards
- elevation of mandible: hinge (inferior synovial cavity)– rotate head of mandible
- depression of mandible: hinge (i**nferior synovial cavity)- rotate head of mandible
- Retrusion: glide (superior synovial cavity)- slide head of mandible posteriorly
- Protrusion: glide (superior synovial cavity)- slide head of mandible anteriorly
How far are you able to open your mouth with the simple motion depressign the mandible? What complex motion needs to occur to open the mouth wider than this?
15 degrees
To open wider need to combine mandible depression with protraction
What happens during TMJ dislocation?
During TMJ dislocation, the head of the mandible travels anterior to the articular tubercle of termporal bone, bettign stuck. This “stuck” position can lock the jaw open
How is the complex motion of moving the jaw side-to-side accompished? What function is this motion important for?
One side of the jaw protracts while the other retracts. The retracted side remains almost stable. This motion is important for chewing.
Name the 3 ligaments of the TMG, their attachmens and functions,

From top to bottom
-
Lateral Ligament:
- Articular tubercle adn neck of mandible
- restricts retraction
- thickening of joint ligament
- Sphenomandibular ligament
- spine of the sphenoid and lingula
- resists protraction adn depression
- Stylomandibular ligament
- styloid process and the posterior portion of the angle of the mandible
- resists protraction adn depression

What nerves innervate the TMJ?
What arteries supply the TMJ?
Nerves: auriculotemporal nerve and massenteric nerve
Arteries: superficial temporal artery and maxillary artery (terminal divisions external carotid)
What muscle is indicated on the provided image?
Attachment points?
Innervation (nerves & arteries)?
Function?

- Masseter
- Attachment
- Origin:
- temporal process of zygomatic bone
- inferior border of zygomatic arch
- Insertion
- Angle of mandible
- lateral surface of mandibular ramus
- Origin:
- Innervation
- Nerves:
- Masseteric nerve (from V3)
- Artery
- Masseteric artery (from maxillary a.)
- Nerves:
- Function: elevate and protract (minor) the mandible
What muscle is indicated on the provided image?
Attachment points?
Innervation (nerves & arteries)?
Function?

Temporalis
- Attachments
- Origin
- inferior temporal line
- temporal fossa
- temporal fascia
- Inerstion
- coronoid process
- anterior margin of mandibular ramus
- Origin
- Innervation
- Nerves
- deep temporal nn (2 total; V3)
- Arteries
- Deep temporal aa. (2 total; from maxillary a.)
- Nerves
- Function
- Elevation and retraction of mandible

What muscle is indicated on the provided image?
Attachment points?
Innervation (nerves & arteries)?
Function?

Medial Pterygoid
- Attachments
- Origin
- Deep Head: medial surface of the later plate of the pterygoid process of the sphenoid
- Superficial Head: maxillary tuberosity or maxilla & pyramidal process of palatine
- Insertion
- (both heads) medial surface of mandible near angle of mandible
- Origin
- Innervation
- Nerves
- Medial pterygoid n. (from V3)
- Arteries
- Medial pterygoid a. (maxillary a.)
- Nerves
- Function: Elevation and protraction (minor)
- forms a sling around angle of mandible with masseter (same function)



