Pathology Lab-Respiratory Flashcards
(56 cards)
A 22-year-old man with diabetes mellitus presented with hemoptysis. He has had insulin dependent diabetes since age 14, was hospitalized for ketoacidosis ages 14 and 19. He has an uncle with type II diabetes, a nephew with type I diabetes, his father has history of asthma as does his mother. His PPD positive and was treated 15 years ago with INH. He reports mild chills, temperature at home 103F and is not eating well last few days. He is a thin, pale male in mild distress; HR 98, RR 24, pO2 90. Labs show WBC 8,900, blood glucose 240, HgA1C 9. Chest radiography shows a cavitary nodular lesion with air-crescent in the right lower lung. He underwent wedge resection of the lesion. What is the top choice in your differential diagnosis?
His history may point you towards a secondary Tb infection. However, his chest x-ray reveals a cavitary lesion in the lower, lung, where secondary Tb usually does not present. This points you towards a fungal infection. Since he is diabetic, he is immunocompromised. Aspergillus is an opportunistic fungal infection and is the top choice in your differential.
An HIV patient presents with a sore throat. Culture of what organisms would give you a hint that the patient is tipping into immunosuppression? How should you that this patient?
Canida albicans infection in the mouth. It is an opportunistic infection and tells you the patient is tipping into immunosuppression. This patient should prophylax with TMP-SMZ (trimethoprim and sulfamethoxazole).
Which fungal infections are pathogenic in immunocompetent patients?
Coccidioidomycoses, Histoplasmosis and Blastomycoses.
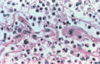
A patient presents to you clinic because a mass was seen in a cavity on his CXR. Biopsy of his lung is shown below. What conditions set him up for this condition?

Bronchiectasis, M. Tb and old abscesses can form cavities and set up a nice place for an aspergilloma.
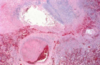
A diabetic patient presents to your clinic with hemoptysis. Biopsy of this lung is shown below. What is causing his symptoms?

Note the many dichotomous branching hyphae with septation and 45 degree angle of branching in the biopsy. This is invasive aspergillus. It gets into the blood vessels and causes bleeding (shown below).
A 19 year old female with a history of asthma comes to see you with worsening of symptoms. Bronchoscopy reveals mucus impaction, dilation of the bronchi and bronchiectasis. What would you expect to see on biopsy of the tissue in her lungs?
Allergic bronchopulmonary aspergillosis. This is a type I hypersensitivity and you would see eosinophil infiltrate and IgE antibodies.
A 59-year-old nurse complained of fatigue, weight loss, night sweats and a productive cough. She has had heavy menses from fibroids for many years, worked on Navajo reservation for 15 years, is post menopausal, on low dose estrogen therapy and had a fever of 101° F at home. Her father died of heart attack at age 75. Her mother 80 yo in good health. She appears thin, tired and pale appearing female. She complains of frequent coughing. Physical exam reveals HR 85, RR 20. A sputum smear showed acid-fast bacilli. A chest X-ray showed fibronodular densities in the left apex. What would a positive PPD tell you in this patient?

She recently acquired Tb, she had it in the past but it’s been eradicated or she has been vaccinated against it. The PPD is just an injection of Tb antigen and looking for a delayed hypersensitivity reaction a few days later. All this indicates is that her immune system has seen Tb before.
What test might you do on a patient who has suspected Tb, but has had a previous Tb vaccination.
IF-gamma release assay. You take a blood sample and add Tb antigens. Overnight incubation will reveal a Th1-induced increase in IF-gamma.
Which of these gross sections is primary and which is secondary Tb?

*

A patient presents with a fever and productive cough with bloody sputum. Sputum culture reveals acid fast bacilli. CXR reveals a cavitary lesion in the apex of his right lung. What accounts for the biopsy of the lesion seen below?

The image is a caseating granuloma that forms with patients infected by M. Tb. Macrophages are activated to destroy to mycobacterium. However, the mycobacterium prevents fusion of the phagolysosome in the macrophage. This causes the macrophage to release TNF-alpha, the Th1 cell to release IF-gamma and other macrophages are recruited to form a granuloma and wall off the infection.
How would your diagnosis differ in each of these patients after seeing their biopsy?

Note the granuloma on the left does not have necrosis. That image could be anything…it just lacks necrosis. The image on the right is definitely not sarcoid because sarcoid does not present with necrotizing granulomas.
How would Tb cause the symptoms seen in the patient below?

It infects the meninges and can cause cranial nerve palsy.
A patient presents with Tb. His radiograph is shown below. What is this condition called?

Note the evidence of vertebral destruction in the classic anterior wedge formation with intervertebral disk involvement. This is Pott’s disease. This is when Tb infects the vertebrae.
A 30-year-old African-American female presents with a persistent cough and joint pains. She is a G2P2, has a history of endometriosis, is currently on OCPs, is unable to play regular tennis and is unable to “catch her breath” and feels tired all of the time. Her father has sickle cell trait, is alive and healthy at age 56. Her mother has osteoarthritis and is 54. She is an alert female in no distress. Vitals are HR 75, RR 17. There are no palpable supraclavicular lymph nodes; joints of hands, knees and ankles are tender to palpation but there is no swelling or deformity. Her PFTs and O2 saturation were normal. Her chest x-ray shows bilateral hilar adenopathy. A bronchoscopic biopsy shows epithelioid non-necrotizing granulomas. What about this case screams sarcoidosis?
Respiratory problems, constitutional symptoms, more common in young African-American females, bilateral hilar adenopathy and non-necrotizing granulomas.
Which T-cell over-activations is the culprit in sarcoidosis?
Uncontrolled activation CD4+ cells that make IF-gamma, initiate a Th1 activation, macrophage activation and non-necrotizing granuloma formation (seen below).

Why do patients with sarcoidosis have hypergammaglobulinemia?
CD4 T cells are also driving mass B-cell production of antibody.
What contributes to most deaths from sarcoidosis?

Note the shrunken, hardness and modularity in the lung. Interstitial fibrosis from chronic inflammation of the lung. Loss of normally thin alveolar-capillary interface is shown below.

A patient presents to your clinic with interstitial fibrosis and bilateral hilar adenopathy. What parts of the patients blood work might be elevated?
These symptoms are highly specific for sarcoidosis. ACE and Ca2+ are elevated in this patient because macrophages in the granuloma can produce ACE and Vitamin D (increasing calcium release into the blood).
A 73-year-old retired insulator gave a history of progressive dyspnea over many years and subsequently presented with right-sided, intractable chest pain and weight loss. He had surgery for rotator cuff tear 5 year ago, rides Harley every weekend but always wears his helmet. During WW II he did extensive repairs to the insulation in the boiler rooms aboard ships. His job as a mechanic had often involved the repair and “regrinding” of brake cylinders. Wife and both parents lifelong smokers. Physical examination disclosed diminished breath sounds, dullness to percussion, a pleural friction rub on the right side and finger clubbing. Labs show pO2 of 90. Why might this patient have increasing dyspnea?
When asbestos fibers get into the lung the macrophages try to digest them. They can’t so you get release of mediators over the years that causes interstitial fibrosis in the lower lobes and dyspnea. Additionally, asbestosis causes mesothelioma which increases secretion of fluid by the mesothelial cells and causes pleural effusion.

What cells would you expect to see in biopsy of the lung in a patient with malignant mesothelioma?
Epithelial and sarcomatoid malignant cells.

What would you expect to see in a biopsy of a patient who has asbestosis?
Dumbbell-shaped asbestos body (ferruginous body) that is heavily coated with iron.

A 55 year old construction worker presents with increasing dyspnea. His CXR is shown below. What would you expect to see on biopsy of the parietal pleura in this patient?

Note the interstitial fibrosis of the lung typically seen in asbestosis. Basket-weaving areas of collagen in the parietal pleura (parietal plaques) are seen on biopsy.

What are the different types of bronchogenic carcinomas?
Small cell (neuroendocrine), large cell, squamous cell and adenocarcinoma.
What is the first distinction you want to make in a patient with bronchogenic carcinoma?
Small-cell carcinoma (must be treated with chemo) and non-small call carcinoma (treated surgically).