Pathology of the Head & Neck Flashcards
(61 cards)
How does the most common aetiology cause the changes described in the stroma?
trauma damaging tissue which can feasibly both directly make vessels leak by structural damage or trigger an inflammatory response which leads to increased vascular permeability
What is the significance of a polyp becoming fibrotic?
rather than being potentially reversible like oedema and fibrin deposition could be, fibrosis is likely to be permanent
it may only be remedied by a surgical procedure
What is the main factor influencing the severity of a polyp?
there are different implications of inflammation and fibrosis depending on the location
it is more life threating in organs such as the heart, liver, kidney or lungs
What are the 3 main lesions of voice abuse?
- vocal cord nodules
- vocal cord polyp
- contact ulcer
these are due to overuse or abuse and are more common in people who use their voice a lot (e.g. professional singers)
What are the main differences between vocal cord polyps and nodules?
nodules:
- usually bilateral
- present on opposing surfaces of the vocal fold, usually on the middle third
polyps:
- >90% are unilateral
- usually in Reinke’s space / ventricular space, usually on the anterior half of the vocal cord
they are clinically different, but histologically similar
What is Reinke’s space?
the part of the vocal cord that lies beneath the elastic lamina
some mucosa in this area is capable of almost intimate expansion
it is a potential space between the vocal ligament and the overlying mucosa
What is a vocal cord polyp?
Who is more commonly affected?
a reactive change of laryngeal mucosa and stroma resulting in benign polypoid or nodular growth
it is caused by vocal abuse and phonation changes
it can occur at any age but is more common in young women
What does a vocal cord polyp look like?
it has a smooth surface and affects the anterior half / anterior third of the vocal cord
it has a translucent appearance (can almost see through it)

What are the histological features of nodules & polyps?
- epithelium is usually unremarkable (normal)
- initially the stroma is edematous, with myxoid matrix
- later the stroma may demonstrate a spectrum of vascular proliferation, hyaline change, or fibrosis
- blood vessels and lymphatics become leaky
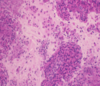
What is shown here?

vocal cord polyp
it is recognised by markedly oedematous stroma underlying a normal epithelium
What is shown here?

vocal cord polyp (late stage)
the polyp may progress to form fibrosis and a solid nodule
fibrin is present
this is plasma that has leaked out of damaged vessels and clotted to form the pink masses
What is the most common aetiology of vocal cord nodules and polyps?
voice abuse, in particular people who use their voice a lot
How can continuous trauma affect the vocal cords?
- trauma can directly damage structures or damage them enough to trigger an inflammatory response
- this leads to vessels becoming more leaky (reversible process as oedema becomes reabsorbed again)
- continuous trauma and inflammation leads to fibrosis
What is the definition of “precursor lesions of laryngeal squamous cell carcinoma”?
What is the problem with identifying these lesions?
squamous lesions with an increased risk of progression to squamous carcinoma
some histologically normal squamous mucosa can be a precursor for dysplasia and invasive squamous cell carcinoma
only 10% of precursor lesions progress to carcinoma
Who is more likely to be affected by precursor lesions of laryngeal squamous carcinoma?
Where are they usually found?
the supraglottic and glottis region are most affected
- peaks in 6th decade
- more common in males than females
- associated with carcinogen exposure - tobacco and alcohol abuse
What is shown here?

low grade dysplasia
abnormal but there is a definite risk of developing invasive carcinoma
What is shown here?

high grade dysplasia
malignant appearing epithelium is confined to the epithelium
there is no evidence of breach of the basement membrane and invasion of underlying tissues
What is a squamous cell carcinoma of the larynx?
What % of cancers does it account for?
a malignant tumour characterised by squamous differentiation
the supraglottic and glottic regions are most affected
it is 1% of all cancers but 90% of all head and neck cancers
Where is squamous epithelium found?
it covers the skin and most of the mucous membranes in the body
it keratinises, flattens off and becomes anucleate and impermeable to water as it becomes more superficial
Who is more likely to get squamous cell carcinoma?
males are much more commonly affected than females
it is associated with tobacco and alcohol abuse
these factors work synergistically
(much more likely to get it if you smoke and drink than if you just smoke and don’t drink)
What is the prognosis like for squamous cell carcinoma of the larynx?
prognosis is dependent on size, site, stage and differentiation
early lesions that are confined to the vocal cord (T1) have a 90% 5 year survival
there is a less than 50% 5 year survival for a T4 lesion
What is shown here?

squamous cell carcinoma
islands of squamous epithelium inflitrating into fibrous connective tissue
it is keratinizing (pink areas are keratin)
How do the 2 most common predisposing factors for laryngeal dysplasia act on the epithelium?
alcohol and tobacco smoke act as carcinogens (synergistically) and the mechanisms for carcinogenesis include:
- activating oncogenes (“foot on the accelerator”)
- inactivating tumour suppressor genes (foot off the brake)
- inhibiting apoptosis (“stopping the car from crashing”)
Why is inhibiting apoptosis a mechanism of carcinogenesis?
when cells show uncontrolled proliferation they may be confined to the basement membrane (“in situ”)
if they keep on proliferating in an uncontrolled way, there is more chance of acquisition of further mutations to enable further “bad” capabilities