Pharm: Cardiac Arrhythmia Flashcards
(101 cards)
1
Q
- What are the three class IA drugs?
A
- Quinidine
- Procainamide
- Disopyramide
2
Q
- What are two class IB drugs?
A
- Lidocaine
- Mexiletine
- (Phenytoin in sketchy)
3
Q
- What are 2 class IC drugs?
A
- Flecainide
- Propafenone
4
Q
- What are 2 class II drugs?
A
- Esmolol
- Propanolol
5
Q
- What are four class III drugs?
A
- Amiodarone
- Ibutilide
- Dofetilide
- Sotalol
“AIDS”
6
Q
- What are 2 class IV drugs?
A
- Verapamil
- Diltiazem
7
Q
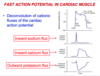
- What is happening during the phases of the fast action potential in cardiac muscle?
A
- Phase 0: voltage-dependent fast Na+ channels open as a result of depolarization; Na+ enters the cells
down its electrochemical gradient - Phase 1: K+ exits cells down its gradient, while fast
Na+ channels close, resulting in some repolarization - Phase 2: plateau phase results from K+ exiting cells
offset by and Ca2+ entering through slow voltage-
dependent Ca2+ channels - Phase 3: Ca2+ channels close and K+ begins to exit
more rapidly resulting in repolarization - Phase 4: Resting membrane potential is gradually
restored by Na+/K+ ATPase and the Na+/Ca2+
exchanger
8
Q
- What is happening during phase 4 of the pacemaker action potential?
A
- phase 4 is a slow spontaneous depolarization
- poorly selective ionic influx of Na, K occurs via If and T-Ca2+ channels, respectively.
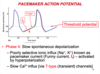
9
Q
- What is happening during phase 0 and 3 of the pacemaker action potential?
A
- Phase 0 is the upstroke of nodal action potential
- Ca+2 influx via the relatively slow (L-type**) (long-acting) Ca2+ channels
- Phase 3 is the repolarization of the nodal action potential
- inactivation of calcium channels with ^K+ efflux

10
Q
- How does the rate of spontatneous depolarization in phase 4 effect firing rate of nodes?
A
- decreased slope–> decreased rate of node because it takes more time to reach threshold potential
11
Q
- How does resting potential effect nodal action potential firing rate?
A
- if potential is less negative, less time needed to reach threshold so the firing rate increases
12
Q
- Where is ERP on the action potential?
- Where is AP on the action potential?
A

13
Q
- What are the three states of sodium channels in the heart?
- in which state do the m-gates open?
- in which state do h-gates close?
A
-
Resting state – the channel is closed but ready
to generate action potential -
Activated state – depolarization to the threshold
opens m-gates greatly increasing sodium
permeability -
Inactivated state – h-gates are closed, inward
sodium flux is inhibited, the channel is not
available for reactivation – this state is
responsible for the refractory period

14
Q
- Class I drugs bind most readily to which states of sodium channels?
A
- Activated or inactivated
- very little affinity towards channels in a resting state
15
Q
- What is the order of sodium channel binding affinity in class I drugs?
A
- CAB
- C has highest affinity (**slowest to dissociate**)
- B has lowest affinity (**quickest to dissociate**)
16
Q
- Which class I drugs has intermediate dissociation kinetics?
A
IA
17
Q
- What does K+ channel blockade do?
A

18
Q
- How is the fast action potential effected by 1A drugs?
- AP length?
- Effective refractory period (ERP)?
- QT interval? Why?
- QRS?
A
- AP duration is increased
- ERP is increased
- QT interval is increased (Class IA also block potassium channels)***
- QRS is prolonged (widened)

19
Q
- What type of cells are preferentially targeted by class IA drugs?
A
- Ectopic pacemaker cells with faster rhythms
20
Q
- Which class IA drug has antimuscarinic and ganglionic blocking effects?
- what can this cause?
A
- Procainamide
- can cause hypotension

21
Q
- What are the indications for procainamide?
- acute therapy vs quinidine?
- long term tx?
A
- PSVT
- prevent recurrence of VT
- treat arrhythmias of MI
- tolerated better than quinidine when given IV as acute therapy
- long-term treatment poorly tolerated

22
Q
- What is the active metabolite of procainamide that has class III activity?
- what patient population can this be worrisome?
A
- active metabolite N-acetylprocainamide has class III activity, has longer half-life, accumulates in renal dysfunction patients
- measurements of both parent drug and metabolite are necessary in pharmacokinetic studies
23
Q
- What are the adverse cardiac effects of procainamide?
A
- Prolongs QT (K channel blockage) which can lead to TdP, although not as likely to cause torsades as quinidine
- excessive conduction block

24
Q
- What are some extracardiac adverse effects of procainamide?
- prolonged use can lead to?
A
- N/V/D, rash, fever, hypotension
- prolonged use can lead to a positive ANA test drug-induced lupus syndrome, especially in slow acetylators
- can cause agranulocytosis

25
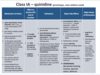
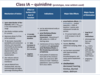
* What is the MOA of quinidine?
* open-state blocker of Na+ channels
* also blocks multiple cardiac K+ channels

26
* Which class IA drug is a natural alkaloid from cinchona bark that has anticholinergic and **alpha-adrenergic _blocking_** effects?
* Quinidine
27
* What are the effects of quinidine on
* QRS duration?
* QT interval?
* Inotropy?
* 10-20% increase in QRS duration
* 25% increase in QT interval
* negative inotrope

28
* What are the indications for use of quinidine?
* afib, aflutter (pharmacological _conversion_) (because Class I are rhythm control drugs)
* maintenance of sinus rhythm in patients with paroxysmal afib/flutter, or life-threatening ventricular arrhythmias
29
* Which drug is associated with decreased hearing, tinnitus, blurred vision, and delirium? What is this called?
* Quinidine
* Cinchonism
30
* Which drug with hypersensitivity reactions, thrombocytopenia, and rarely severe hepatotoxic reactions?
* Quinidine

31
* Which class IA drug is likely to put you in a normal rhythm, but also 2-3x more likely to kill you?
* Qunidine, the prototype class IA drug, which is now seldom used

32
* What is the MOA of disopyramide?
* what effect does it have on peripheral vessels?
* blocks Na channels similar to quinidine
* is NOT an alpha-adrenergic receptor antagonist like quinidine, instead is a peripheral vasoconstrictor

33
* How does disopyramide effect
* QRS?
* QT?
* Inotropy?
* prolongs QRS
* prolongs QT
* negative inotrope

34
* What are the indications for disopyramide?
* offlabel use?
* used to prevent recurrence of vtach or vfib
* maintains sinus rhythm in pts with afib/flutter
* off label use: maintenance of sinuys rhythm in afib patients that have vagally-induced afib or hypertrophic cardiomyopathy

35
* Which class IA drug exerts the most anticholinergic side effects?
* what are these side effects?
* Disopyramide
* dry mouth, blurred vision, constipation, urine retention, closed-angle glaucoma\*\*

36
* Which class IA drug is used to convert supraventricular tachycardias such as WPW when given in IV form
* how does this work?
* procainamide
* inhibits conduction in the accessory pathway

37
* Which drug is indicated for vagally mediated afib?
disopyramide
38
* What does the action potential look like when a patient is given a class IB drug?

39
* What effect do class IB drugs have on sodium and potassium channels?
* which state of sodium channels do they bind to?
* State-dependent sodium channel blockage
* binds to inactivated sodium channels
* preferentially depolarized cells--\> **ischemic damage** causes depolarization of cells due to loss of ATP
* 1B drugs DO NOT block K+ channels and thus do not (usually) significantly prolong action potential, QT duration.

40
* What is the MOA of lidocaine?
* blocks both the initiation and conduction of nerve impulses by decreasing the neuronal membrane's permeability to sodium ions
* (konorev mentions only inactivated na channels, while wolff says both open and inactivated)

41
* Which drug is (\*used to be\*) indicated for the acute IV therapy of ventricular arrhythmias?
]
* lidocaine

42
* Which drug is for use in Advanced Cardiac Life Support (ACLS) situations in which _amiodarone is not available_ for hemodynamically stable or monomorphic/polymorphic VT, and for _pulseless vfib_ that is _unresponsive to defibrillator, CPR, and vasopressor administration_?
* Lidocaine

43
* Which two class I drugs are likely to cause dizziness, paresthesia, altered consciousness, coma, seizures, etc? (CNS effects)
* Class IB
* Lidocaine, Mexiletine

44
* Which class I drug must be given IV due to extensive first-pass metabolism by CYP3A4?
* Lidocaine

45
* Which class IB drug can be given orally?
* mexiletine

46
* which class I drug is indicated for use only to treat_sustained ventricular arrhythmias, but does NOT appear to prolong life?_
* mexiletine

47
* Which CYPs eliminate Mexiletine?
* CYP1A2
* CYP2D6

48
* what is first line therapy for ischemia induced ventricular arrhythmias?
* Amiodarone
49
* Which class IB drug is indicated for use to relieve chronic pain, especially pain _due to diabetic neuropathy and nerve injury?_
* Mexiletine
50
* What does the fast action potential look like due to class IC drugs?

51
* What is the MOA of class IC drugs?
* effect on sodium channels?
* which state of sodium channel?
* kinetics?
* effect on QT? QRS?
* Block sodium channels, slow conduction in cardiac tissue
* preferentially bind to open (activated) state
* slow kinetics
* block some potassium channels
* do NOT prolong AP or QT interval
* do prolong QRS interval

52
* Which _class I drug_ is ideal for use in those with _catecholaminergic polymorphic vtach?_
* flecainide

53
* What are the clinical uses of flecainide?
* maintenance of sinus rhythm in patients w/ _paroxysmal supraventricular arrhythmias in whom **structural heart disease is absent**_
* life threatening ventricular arrythmias, such as sustained vtach, in patients who **don't have structural heart disease**

54
* Flecainide can be proarrhythmic, especially in patients who have had which three contraindications?
* patients w/ preexisting vtach
* patients w/ previous infarction
* patients w/ ventricular ectopic rhythms

55
* Which class IC drug has weak beta blocking activity?
* propafenone
56
* What are the clinical uses of Propafenone?
* used to maintain sinus rhythm in patinets with SVT (including afib)
* in patients with _disabling symptoms and without structural heart disease_
* in sustained ventricular arrhythmias in patients with _disabling symptoms and without structural heart disease_

57
* What are some adverse effects of propafenone?
* Exacerbation of ventricular arrhythmias
* _metallic taste_
* _constipation_
* **exacerbation of asthma** (some beta-blockade activity)

58
* What should you not combine propafenone with?
* do not combine with the CYP2D6 and CYP3A4 inhibitors as the risk of proarrhythmia may be increased

59
* Overall, what are the indications for use of class IC drugs?
* afib in structurally normal heart
* svt, including avnrt, avrt, and atrial tachycardia
* particularly effective at _inhibiting reentrant tachycardia using accessory pathways_

60
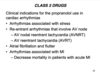
* good summary of class I drugs

61
* What is the effect of class II drugs on the nodal potential?

62
* How do beta-adrenoceptors work in the heart in the absence of a beta-blocking drug?
* this was implied in the DSA and I didn't know it, so found another source.
* coupled to a Gs protein, which activates AC to form cAMP from ATP
* increase cAMP activates PK-A, which phosphorylates L-type Calcium channels, causing _increased calcium **entry into the cell**_
* increased calcium entry leads to enhanced release of calcium by the sarcoplasmic reticulum. this increases inotropy (contractility) of the heart and also chronotropy.
* PK-A also phosphorylates other sites on SR that lead to enhanced release of calcium through ryandodine receptors, providing more calcium for binding troponin C--\> increases inotropy
* lastly, PK-A can phosphorylate myosin light chains, which also has positive inotropic effects

63
* What is the MOA of class II antiarrythmics?
* block sympathetic stimulation of primarily Beta 1 receptors, which decreases cAMP, decreases inward Ca2+ currents, thus suppressing abnormal pacemakers by decreasing the slope of phase 4

64
* What are the indications for use of propranolol in cardiac arrhythmias?
* Arrythmias associated w/ stress
* AVNRT, AVRT
* Afib/flutter
* Arrythmias associated with myocardial infarcts
65
* Which class II drug has a half-life of 10 minutes because of hydrolysis by blood esterases?
* esmolol
66
* How is esmolol given?
* what is its MOA?
* used as continuous iv infusion, with rapid onset and termination of its action
* short acting _selective_ beta-1 blocker
67
* What are four indications for the use of esmolol?
* Supraventricular arrhythmia
* Arrythmia associated with **thyrotoxicosis**
* Myocardial ischemia or acute MI with arrhythmias
* as an adjunct drug in general anesthesia to **control arrhythmias in perioperative period**

68
* There are a plethora of adverse effects of class II drugs; how do they effect the following:
* cardiac output
* asthma
* liver glucose mobilization
* lipid profile
* consciousness
* sexual effect
* what happens if you lose your bottle of beta blockers and can't get anymore?
* Reduced cardiact output
* bronchoconstriction
* impaired liver glucose mobilization
* increase VLDL, decrease HDL
* sedation, depression
* impotence
* rapid withdrawal produces **rebound hypertension**

69
* What are the (six) contraindcations for use of class IIs?
* konorev loves this shit
* athma
* peripheral vascular disease
* raynauds
* T1 DM patients on insulin
* bradyarrythmias and AV conduction abnormalities
* severe depression of cardiac function

70
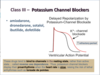
* How do Class III potassium channel blockers effect the fast action potential?

71
* Which class of antiarrythmics bind to channels in the **resting state**, thus exhibiting **reverse use dependence** (display their proarrhythmia when HR is slow, raising _risk of lethal arrhythmias such as TdP?_
* Class III- Potassium channel blockers
72
* Which potassium channels are opened during the phase 4?

* Inwardly rectifying K+ channels

73
* What are the effects of class III drugs on:
* AP
* QT interval
* ERP
* Prolong AP
* Prolong QT
* Prolong ERP
* dont change QRS because phase 0 isnt effected

74
* Which class III drug does _not show reverse-use dependence_
* _aka refractoriness is not increased at slow HRs_
* Amiodarone

75
* Which class III drug blocks inactivated sodium channels and possesses adrenolytic activity? (alpha,beta blocking properties)
* Amiodarone
* alpha blocking causes peripheral vasodilation, i think

76
* What are the indications for use of amiodarone?
* **oral therapy** in patients w/ recurrent vtach or vfib? resistant to other drugs
* maintaining sinus rhythm in patients w/ afib

77
* What are four major side effects of amiodarone?
* what side effect does Amiodarone NOT have that other class III medications do?
* Pulmonary fibrosis
* hyperthyroidism or hypothyroidism
* corneal micro-deposits
* bluish discolaration of the skin
* \*\* does not cause torsades\*\*

78
* If you stop amiodarone, how long are its effects maintained?
* how long is half life
* half life is around 50 days, but metabolites can be found in tissues 1 year after discontinuation

79
* How would rifampin (tb drug) effect amiodarone?
* How would cimetidine effect amiodarone?
* rifampin is a CYP3A4 inducer, so it would decrease the half-life of amiodarone
* cimetidine in a CYP3A4 inhibitor, so it would increase the half-life of amiodarone

80
* What should be specifically monitored in patients on amiodarone due to its side effects?
* three tests
* LFTs due to hepatotoxicity
* PFTs due to pulmonary fibrosis side effect
* TFTs due to amiodarone being 40% iodine by weight which can cause both hypo or hyper thyroidism
81
* Which class III drug also shows some class II activity?
* non-selective beta-blocker
* Sotalol

82
* What are the indications for the use of sotalol?
* life-threatening ventricular tachyarrhythmias
* maintenance of sinus rhythm in patients w/ afib

83
* What are some adverse effects of sotalol?
* same as beta blocker--\> depress cardiac function
* provokes TdP
84
* Which class III drug specifically blocks _the rapid component of the delayed rectifier potassium current, thus its effect is more pronounced at lower HRs?_
* __delayed rectifier potassium channel is IKr

* dofetilide

85
* Which class III drug is used for conversion of AF to sinus rhythym and maintenance of sinus rhythm after its been converted?
* dofetilide

86
* Which class III drug must have its dose modified in kidney failure patients based on the Creatinine clearance ?
* dofetilide

87
* Which class III drug is infused intravenously for **acute afib or flutter** for conversion to NSR?
* ibutilide

88
* After converting a patient's acute afib back to NSR with ibutilide, should you let them get up and leave?
* No, must monitor EKG continuously until QTc returns to baseline

89
* Which class III drug is indicated for arrhythmias that are acute, or have short duration?
* also used for converting cardiac surgery induced afib, and in WPW syndrome (accessory pathway arrhythmias)
* ibutilide

90
* Which class III drug is indicated for prevention of recurrent afib or vtach due to an old mi?
* sotalol

91
* Which class III drug can be used in CHF patients and why?
* Dofetilide because it is not a negative inotrope due to its pure action on IKr channels

92
* how do class IV drugs effect the nodal action potential?
* note threshold is increased

93
* What is the MOA of class IV drugs?
* which state/type of channel?
* slope of phase 0
* threshold potential
* refractory period in AV node
* Block both activated and inactivated L-type calcium channels
* decrease slope of phase 0
* increase L-type calcium channel threshold potential
* prolong refractory period in AV node

94
* How do class IV drugs effect conduction velocity and PR interval?
* decrease conduction velocity
* increase PR interval
95
* What are the clinical indications for verapamil and diltiazem?
* termination of supraventricular tachycardias and prevention of recurrence
* ventricular rate control in afib/flutter

96
* What are some cardiac and non cardiac side effects of class IV drugs?
* CHF due to negative inotropy
* bradycardia
* hypotension
* heart block
* SA node arrest
verapamil can cause constipation\*\*

97
* What are two MOAs of adenosine?
* Activates potassium curent and inhibits Calcium and funny currents, causing **marked hyperpolarization** and suppression of action potentials in slow cells
* inhibits av conduction and increases nodal refractory period

98
* What is the name of the GPCR that adenosine binds to?
* A1 adenosine receptor
99
* What are two clinical indications for adenosine?
* rapid IV bolus for the acute termination of **re-entrant SVT**
* also used to induce controlled hypotension

100
* What drug likely caused this?

* adenosine
* produces a transient asytole/AV block
101
* What are some side effects of adenosine?
* Chest fullness, burning sensation
* AV block
* Rarely triggers bronchospasm due to A1/A2B adenosine receptors causing bronchoconstriction
* hypotension
* impending doom, cutaneous flush (sketchy)


