Pulmonology Flashcards
(48 cards)
Most common CAP Pediatric patients
Pediatric patients
• Age 4 mo to 4 yrs
– Most common pathogen
• RSV
– Peak incidence • 2-7 mo of age
• Age 5-18 yrs
– Most common pathogen • Mycoplasma pneumoniae – Treat with a macrolide
Score for Pneumonia Severity
Estimates mortality of community-acquired pneumonia to help determine inpatient vs. outpatient treatment.

CAP Treatment for Outpatient, previously healthy, no risk for DRSP infection
Outpatient, previously healthy, no risk for DRSP infection
– Macrolides (SOR A) • Azithromycin • Clarithromycin • Erythromycin
OR
– Doxycycline (SOR B)
CAP treatment for Outpatient with comorbidities or recent abx

CAP treatment for Inpatient (Non-ICU)
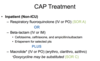
CAP treatment for Inpatient (ICU)

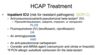
HCAP Treatment - Outpatient or inpatient

HCAP Treatment - ICU
Pneumococcal Vaccines
PPSV23—Pneumococcal Polysaccharide vaccine (Pneumovax)
– 23 serotypes that cause 80% of invasive pneumococcal disease in US – B-cell response – 96% drop in pneumonia caused by susceptible strains
PCV-13—Pneumococcal Conjugate vaccine (Prevnar 13)
– T-cell response
Conjugate Vaccine (PCV13)
- Primary series 2, 4, 6 months, booster 12-15 months
- All adults > 65
- Adults > 19 with CSF leaks, cochlear implants, functional asplenia or immunosuppression
Polysaccharide Vaccine (PPSV) 23

How to Give Both PCV13 and PPSV23
CDC now recommends 2 pneumococcal vaccines for adults >65 years
- Age 2-18– Give 1 dose of PPSV23 at least 8 weeks after the final dose of PCV13. (If immune compromise or asplenia, should receive a 2nd dose of PPSV23 5 years after the first PPSV23)
- Age 19-64 at high risk – give PCV13 first followed by PPSV23 at least 8 weeks later
- Age > 65 give PCV13 first, followed by PPSV23 6 to 12 months later (min 8 weeks if immunocompromised)
- If your patient has received any doses of PPSV23, the dose of PCV13 should be given at least 1 year later

TB Skin Testing > 5 mm is considered positive if:
- HIV sero-positive
- Recent TB direct contact
- CXR shows prior inactive TB
- Immunosuppressed patients – Prednisone > 15 mg/day – TNF-a antagonists – Organ transplant recipients
TB Skin Testing
> 10 mm is considered positive if:
Long-term care facility – Resident or employee • Inmate • IV drug user • Children < 4 yrs of age • Mycobacteriology lab personnel • Diabetic • Renal failure • Cancer • Recent immigrant (< 5 yrs) from high-risk country • High-prevalence area
TB Skin Testing > 15 mm is considered positive if:
• Any person with no known risk factors – Even if prior BCG vaccination
Booster Phenomenon
- Some people infected with M. tuberculosis may have a negative reaction to the TST if many years have passed since they became infected.
- They may have a (+) reaction to a subsequent TST because the initial test “stimulates” their ability to react to the test. – This may incorrectly be interpreted as a skin test conversion
- The two-step test is indicated for serial testing situations, to avoid thinking that this latent “wake up” is a new infection or conversion
Two-Step Skin Testing

Workup of Positive TST or IGRA
- Check CXR for active disease – If CXR Negative (latent tuberculosis)
- Isoniazid (INH) for 6-9 months (9 mo is preferred) – Daily or intermittently (twice weekly) – Use directly observed therapy (DOT) for intermittent regimen
- Rifampin daily for 4 months, consider adding Pyridoxine
- Monthly exams for signs of hepatitis and medication adherence, check liver transaminases if indicated
Workup of Positive TST or IGRA
- If CXR positive (Active tuberculosis)
- Aggressive Combination therapy indicated to decrease mortality, transmission, and resistance • Four-drug treatment initially: – Isoniazid (INH) – Rifampin (RIF) – Ethambutol (EMB) – Pyrazinamide (PZA)
- Treatment regimen modified once culture results received
Post-Treatment Follow-Up
Regardless of whether Rx for LTBI was completed, serial or repeat CXRs are not indicated unless signs or symptoms of TB develop
Fungal Lung Infections
Opportunistic (more likely in immunocompromised)
• Aspergillosis • Candidiasis
Endemic (farm workers, etc)
- Mississippi/Ohio Valley: Histoplasmosis and Blastomycosis
- Southwest: Coccidiodomycosis
What percentage of airway reversibility and change in FEV1 do you need in order to confirm the diagnosis of asthma?
12% and 200 mL
Spirometry in Asthma
- FEV1 is decreased to < 80% predicted
- TLC is normal to elevated • FRC is usually elevated • Significant reversibility after inhaling a SABA – Increase by ≥ 12% and – 200 mL in FEV1

Asthma Classification – NHLBI

Asthma During Pregnancy
- Albuterol is the preferred SABA
- ICSs are preferred controller medication – Budesonide has the most reliable safety profile
- Comorbid allergic rhinitis can be managed with intranasal steroids






