Random Facts Flashcards
Random Facts leading upto finals (78 cards)
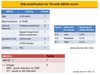
What drugs are used in Migraine Prophylaxis?
Propranolol is used as prophylaxis, as is atenolol. Amitriptyline has been shown to be effective in some patients and is useful in co-morbid depression. Pizotifen is used in migraines as prophylaxis. Diclofenac may be used as acute treatment, but not prophylaxis. Rizatriptan and other triptans are used only in acute attacks.
How do you differentiate between viral meningitis and encephalitis?
The crucial difference between viral meningitis and viral encephalitis is that impairment of brain function which should be completely absent in viral meningitis.
Does LMWH cross the placenta and are they safe in breastfeeding?
LMWHs do not cross the placenta and is not orally active so is safe in breastfeeding mothers
How do you reverse LMWH and unfractionated heparin
Although anticoagulation with unfractionated heparin can be reversed by protamine sulphate, there is no way of reversing LMWH.
What are the most common causes of osteolytic and osteoblastic bone metastases?
The most common causes of osteolytic bone metastases in an adult include lung, breast, thyroid, kidney and colon cancer. The most common causes of osteoblastic metastases in an adult include prostate (male) and breast (female).
HBV is chronic when present for how long?
6 Months
Which wrist # is also known as a dinner fork deformity and where is the distal fragement displaced too?
Colle’s # with dorsal displacement. As opposed to Smith’s # which has a palmar displacement.
A FOOSH will most commonly cause what type of wrist #.
What will cause the other type of wrist #
Collie’s
Falling onto a flexed wrist

Childhood Vaccine Schedule?
2 months – DPT/polio/Hib + pneumococcal conjugate vaccine (PCV)
3 months – DPT/polio/Hib + MenC
4 months – DPT/polio/Hib + MenC + pneumococcal conjugate vaccine (PCV)
12 months – Hib/MenC
13 months – MMR + pneumococcal conjugate vaccine (PCV)
3-5 years (pre- school) – MMR II/ DTP / Polio
13-18 years (school leavers) – Diptheria/ Tetanus/ Polio (not Pertussis)
Barrett’s Oesophagus is a risk factor for which type of cancer
Oesophageal Adenocarcinoma
Tell me about NNH and Maternal HSV
NNH is rare but when it occurs it has a high neonatal mortality rate and requires immediate treatment. The risk of NNH is highest if the mother acquires HSV for the first time during pregnancy, this is because she may not have had opportunity to develop maternal HSV antibodies that can cross the placenta and confer immunity to the baby before he or she is born. In the 1st and 2nd trimester, recurrences should be managed as they are in non-pregnant patients. Aciclovir is not licensed in pregnancy but there is substantial clinical experience supporting its safety. HSV outbreaks in the 3rd trimester are potentially more concerning, as there is a high risk of viral shedding during labour. Recurrences during the 3rd trimester should be managed as per non-pregnant patients and continuous aciclovir can be considered in the last 4 weeks of pregnancy to reduce the risk of clinical recurrence at term, subsequent risk of neonatal transmission and the need for caesarean section. However, if there is a high suspicion of primary HSV infection in the 3rd trimester then caesarean section should be considered to minimise the risk of neonatal transmission.These cases should be discussed with the obstetric/paediatric team.
Is there a hep A vaccine?
Hepatitis A vaccine can be given up to 14 days after exposure providing exposure was within the infectious period of the source case (i.e. during prodromal illness or first week of jaundice). Human normal immunoglobulin (HNIG) intra-muscularly (IM) can be considered for patients at higher risk of complications: concurrent hepatitis B or C, chronic liver disease or age over 50 years. It is most effective if given in the first few days after first contact, with an efficacy of 90%. It is unlikely to give any protection more than 2 weeks after first exposure but may reduce severity if given up to 28 days after exposure.
What is the Stamford Classification?
According to this classification, what is the difference between a Type A and B?
Classification of Aortic Dissections
Type A is ascending and more severe
Type B is descending and less severe
What is the Child-Pugh Score?
The Child-Pugh score is often used to assess the clinical state of patients with cirrhosis of the liver and to indicate the severity of the condition.
What are the radiographic changes associated with bronchiectasis?
Thickened bronchial walls
Ring shadows (thickened airways seen end-on)
Volume loss secondary to mucous plugging
Air-fluid levels may be visible within dilated bronchi
Causes off bronchiectasis?
Congenital/Hereditary: Cystic fibrosis, Ciliary dyskinesia, Marfan’s syndrome, alpha1-antitrypsin deficiency
Post infection: Pneumonia, measles, tuberculosis
Obstruction: Tumour, nodes, foreign body
Inhalation/aspiration
Allergy: Allergic bronchopulmonary aspergillosis
Pulmonary fibrosis: Not usually visible on chest X ray but is seen on high resolution CT scanning with bronchiectasis in areas of fibrosis
Immunodeficiency states: eg AIDS – usually as a result of recurrent infection
Miscellaneous: Rheumatoid-arthritis-associated lung disease, Sarcoidosis, Bronchiolitis obliterans
what is the drug of choice for penicillin-allergic patients with uncomplicated community-acquired pneumonia?
clarithromycin
Is Gentamicin good against aerobic or anaerobic bacteria?
Gentamicin is inactive against anaerobes (and Streptococcus pneumoniae).
How do you identify between Large and Small Bowel Obstruction?
Small bowels will have mucosal folds spanning the width of the bowel known as valvulae conniventes. Large Bowel will have mucosal folds that do not span the entire width of the bowel known as Haustra.

What do the antibodies ASMA and AMA stand for and what diseases are they found in?
Anti-smooth muscle antibodies and antimitochondrial antibodies are typical of autoimmune hepatitis and primary biliary cirrhosis respectively
What antibiotic is used to treat Giardia lamblia
Oral Metronidazole
What are the ECG changes associated with LV hypertrophy?
ECG changes showing LV hypertrophy include:
Prolonged QRS (broad)
Tall R wave (>5 squares)
Left axis deviation
Inverted T waves in V5/ V6 (if severe).
How do post-MI left ventricular aneurysms present?
ST elevation on ECG, pain and arrhythmias, although they may rupture with shock and rapid demise.
Do you know about Scleroderma
Yes or No