Renal 1: Introduction to the kidneys --> from blood plasma to urine (filtration) Flashcards
What are the 4 functions of the kidneys?
- Regulates the extracellular fluid (ECF)
- Acid-base balance (maintenance of pH)
- Waste disposal
- Hormone production
How is the ECF regulated?
- ECF volume
- Water & Na+balance
- Electrolyte composition
- Na+, Cl-, K+, Ca2+, H+ (pH= acidic), bicarbonate, phosphate, sulfate, magnesium
- Osmolarity
- 300 mOsm/L (needs to maintain this)

What is waste that needed to be disposed thorough the kidneys?
Waste disposal –Eg. Urea & foreign compounds (drugs etc)
What are the hormones that are produced by the kidneys?
Erythropoietin (production of red blood cells), renin (blood volume), vitamin D activation (vit. D for blood Ca+)
Urine _____ varies as the kidneys maintain homeostasis
composition Eg. eat salty –> get rid of salt –> pee out salt
What is the structure of the renal system?

Where are the kidneys located?

The ___ kidney is lower than __. Why?
R; L
make space for the liver (which takes up a lot of space)

Kidneys are _____ (intra/retroperitoneal). What does that mean?
retroperitoneal behind the peritoneal cavity- surround by fat and connective tissue (“retro”= behind)

What is the structure of the kidney?

What are the 5 main structures of the kidney
- Outer cortex
- Renal pyramid (inner medulla)
- Calyces
- Renal pelvis
- Ureter

Where does urine travel from? (start in the renal pyramids)?
- Urine drains from renal pyramids into calyces into renal pelvis (dilated part)
- Urine leaves via the ureter

The renal system is __ (highly/lowly) vascularised? Why?
very highly vascularised- due to function for homeostasis

The kidneys make up < 0.5% body weight, but receive ______ of the cardiac output
20%

What is the nephron?
- (smallest part of kidney that carries out function- where urine is being produced)
- Functional units of the kidneys

What are 3 structures are found in the nephron?
- Renal corpuscle (filtered)
- Renal tubule
- Collecting system (–> ureters)

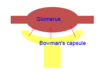
What happens at the glomerulus?
capillary bed- where blood is filtered

What happens at the Bowman’s capusle?
(funnel/cup- being captured)

What is the proximal tubule?
closest to renal corpuscle convoluted

What is the sequence of urine flowing in the nephron to the collecting duct (to the ureter)?
- Glomerus
- Bowman’s capsule
- Proximal convoluted tubule
- Loop of Heenle
- Distal tubule
- Collectig duct
- Ureter

What are the 2 types of nephrons?
- Cortical nephrons
- Juxtamedullary nephrons

What are 3 characteristics of cortical nephrons?
- 80%
- Short loop of Henle
- Mostly in cortex (sit very high up/to the surface of kidney)

What are 3 characteristics of juxtamedullary nephrons?
- 20%
- Long loop of Henle
- Dips deep into medulla

What are the juxtamedullary nephrons important for?
Important for balance Na+ and H20