Respiratory physiology Flashcards
(109 cards)
Whats the biochemical definition for cellular respiration?
The process in which nutrients are converted into useful energy in a cell
Whats the physiological defintion for gaseous exchange?
The process by which an organism exchanges gases with its environment- process and regulation
Whats are the roles of the respiratory system?
and how do these things occur?
- gas exchange
- regulation of blood (tissue) PH: altered by changing blood CO2 levels
- voice production: movement of air past vocal fold makes sound and speech
- Olfaction: smell occurs when airborne molecules are drawn into nasal cavity
- protection: against particles/ microorganisms by preventing entry and removing them
Label the respiratory system…


What are the two zones the respiratory system has and what included in these systems?
1. Conductive zone
- URT (upper respiratory tract)
- Tracheobronchial tree
2. Respiratory zone
- Resoiratory bronchioles to alveoli
- Site for gas exchange
Whats the roles of the nasal cavity?
- passage for air
- cleans the air
- humidifies, warms air
- smell
- acts along with paranasal
- sinuses (resonating chambers)
Whats the structure in the nose that causes turbulalce? What does this mean for keeping the nose/body healthy?
The Conchae causes turbulance of air (gives large surface area)
large particles are blocked from coming in
What do sinuses help with?
- lighten skull
- protection
Whats the pharynx and what are the regions of it?
The Pharynx is a common opening for digestive and respiratory systems
the three regions of the pharynx are;
- Nasopharynx
- Oropharynx
- Laryngopharynx
What are the functions of the larynx?
- maintain an open passageway
- Epiglottis and ventricular folds prevent swallowed material from moving into larynx
- vocal folds are the primary source of sound production
What are the unpaired cartilages of the larynx?
The thyroid, cricoid and epiglottis
What are the paired cartilages of the larynx?
The arytenoid, corniculate and cuneiforms
Whats the functions of the tracheobronchial tree ?
What must we ensure for correct function?
Functions:
- passageway for air movement
- ciliated for the removal of debris
For the correct function to occur you must ensure:
- Theres limited turbulance
- minimal size (dead space)
What does the trachea branch into and where does this lead?
Where is cilia lost in the traceobroncial and why?
The trachea branches into 2 bronchi, one to each lung
In the terminal bronchiole you lose the ciliated epithelium and get squamous epithelium instead which allow for gaseous exchnage with the blood
Label the alveoli?


Tell me the types of cells found in the alveoli and some of the properties/ roles?
1. Type 1 alveolar cells (septal cells)
- in contact with capillary
- simple squamous cells where gaseous exchnage occurs
2. Type 2 alveolar cells
- free surface has microvilli
- secrete alveolar fluid which contains surfactant
3. Alveolar dust cells
- macrophages also found in alveoli to remove debris
The lungs ‘float’ in the thoracic cavity because they are surrounded by a thin layer of what?
pleural fluid
Is the lung directly attached to any muscle?
no
The continual transfer of fluid into the lymphatic channel maintains a negative pressure between what?
The visceral surface of the lung pleura and the parietal pleural surface of the thoracic cavity
Label the muscles that are used for ventilation?


What are the passive elements of ventilation?
- elastic return in lungs
- elastic recoil of ribs
- surface tension in lungs
Whats are the types of pressure in the lungs and where are they found?
- Pleural pressure: pressure in the intrapleural space (always a slightly negative pressure)
- Alveolar pressure: pressure inside the lung alveoli
- Transpulmonary pressure: alveolar pressure- pleural pressure (force that tends to distend the alveoli)
Describe the changes in pressure in the lungs during inspiration and just after?
- the Barometric air pressure (PB) is equal to alveolar pressure (Palv) and there is no air movement
- increases thoracic volume results in increased alveolar volume and decreases alveolar pressure
- Barometric air pressure is greater than alveolar pressure and air moves into the lungs
- End of inspiration
- Decreased thoracic volume results in decreased alveolar volume and increased alveolar pressure
- alveolar pressure is greater than barometric air pressure, and air moves out of the lungs
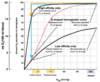
Whats meant by compliance of the lungs?
Name some conditions that decrease the compliance
the ease in which the lungs and thorax expand
conditions which decrease the compliance: pulmonary fibrosis and pulmonary oedema (fluid in the lungs)