REVIEW 3 (cardiac) Flashcards
(30 cards)
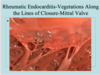
Does the following describe the valvular lesions in RHD or the vegetations seen in Infective Endocarditis?
– larger vegetations along the lines of closure of the valve leaflets.
-No bacteria w/in the vegetations
-ongoing inflammation leads to destruction of valves–> scarring–> valve deformities
RHD
What is “Fish-Mouth Stenosis” and what dz is this seen in?
- Seen in RHD
- The chordae tendinae inserting into the mitral valve are typically shortened and thickened and becomes fused to one another. This fibrous adherence across the commissures of the valve produce a “Fish-Mouth Stenosis”.

Which dz?
Characterized by colonization or invasion of the heart valves, leading to formation of bulky, friable vegetations composed of thrombotic debris and bacterial organisms
Infective Endocarditis
Which disease?
Produces necrotizing, valvular lesions with chance of perforation of the valve
Acute Bacterial Endocarditis
Which condition is a murmur more common due to larger size of vegetations/leaflet destruction and therefore embolization is more likely to occur?
Infective Endocarditis
ABE (Acute bacterial endocarditis) or SBE(subacute bacterial endocarditis)?
______=fever is usually low-grade, along with fatigue and flu-like symptoms
______=quick onset along with chills, night sweats, and weakness.
___SBE___=fever is usually low-grade, along with fatigue and flu-like symptoms
__ABE____=quick onset along with chills, night sweats, and weakness.
ABE or SBE?
- highly destructive infection of the valves.
- Frequently of a previously normal heart valve.
- Also seen in prosthetic heart valves.
- Usually due to Staph aureus or the Gram negatives
- can lead to death w/in days, despite antibiotics.
- Develops in the course of intense bacteremia.
- Produces necrotizing, valvular lesions with chance of perforation of the valve
ABE (Acute Bacterial Endocarditis)

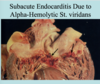
ABE or SBE?
- slower, less virulent disease
- caused by organisms of less virulence (i.e. St. viridans)Can cause infection in previously abnormal heart valves.
- longer course: weeks to months
- most patients recover after appropriate abx therapy.
- The lesions are less destructive and show evidence of healing.
SBE
Which is worse, ABE or SBE? Why?
ABE
- Highly destructive
- Can lead to death w/in days despite abx
- Produces necrotizing, valvular lesions with chance of perforation of the valve
RHD causes ______, involving all 3 layers of the heart
- Pericarditis (fibrinous, “bread and butter”)
- Myocarditis (usually dilated, histology shows Aschoff bodies)
- Endocarditis (most prominent changes seen in valves of the L heart)
Pancarditis
(Per google: Pancarditis is the inflammation of the entire heart: the epicardium, the myocardium and the endocardium)
_________ is a neurologic disorder characterized by involuntary movements that are continuous, non-repetitive, purposeless, jerky movements of the limbs, trunk and face muscles.
Causes impaired speech and gait .
Sydenhams Chorea (extracardiac finding in RHD)
What characteristic lab finding in RHD provides concrete evidence that there has been a recent infection with St. pyogenes
Increasing titers of serum antibodies to Group A Strept antigens (ASO titer)
What disease is an increased ASO titer a characteristic lab finding of?
RHD
What is C-reactive protein (CRP) and what disease is it a characteristic laboratory finding of?
Indicative of an inflammation
Characteristic lab finding in RHD
Causes of what cardiomyopathy?
- Can be primary (idiopathic or genetic):
* genetic: usually autosomal dominant (autosomal and sex linked recessive have also been seen )
Dilated cardiomyopathy
Causes of which cardiomyopathy?
- Secondary causes:
- Toxic w/ ethanol as most common in the U.S. followed by Adriamycin and Cytoxin (Anticancer drugs), long-standing Cocaine use and Cobalt exposure
- Viral Myocarditis
- Pregnancy
- High Catecholamines (pheochromocytoma)
Secondary Dilated Cardiomyopathy
What are the 3 types of cardiomyopathies?
- Dilated Cardiomyopathy
- Hypertrophic cardiomyopathy
- Restrictive cardiomyopathy
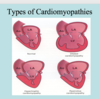
Which cardiomyopathy?
- progressive chamber dilation and systolic dysfunction
- reduced ejection fraction of <25%.
- most common of the 3 CMs
Dilated cardiomyopathy
Which CM?
- multiple secondary causes including alcohol induced, viral myocarditis, and anticancer drugs such as Adriamycin (cardiotoxic drug).
- Morphology reveals a heavy heart which is large and flabby with dilation of all chambers
Dilated cardiomyopathy

Which cardiomyopathy is most common?
Dilated Cardiomyopathy
Gross and microscopic findings of which CM?
- walls are thin, partially replaced by fibrous tissue
- heart size is 2-3x normal
- Coronary arteries usually normal
Dilated Cardiomyopathy
Which CM?
- extensive hypertrophy of the LV myocardium.
- possible left ventricular outflow tract obstruction
- usually asymmetrical thickening of the ventricular septum as compared to the left ventricular free wall
-“Banana shaped” septum
- +/- endocardial thickening with mural plaque formation of the outflow tract.
Hypertrophic cardiomyopathy

Which CM?
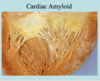
- Decreased ventricular compliance–> results in impaired ventricular filling during diastole with normal systolic function.
- cause can be idiopathic
- can be associated with an abnormal infiltrate such as Amyloid, Sarcoidosis, or metastatic tumor.
- Radiation fibrosis also a cause
Restrictive Cardiomyopathy