Session 2: Blood and Lymph Systems Flashcards
(41 cards)
Describe the external jugular vein and internal jugular vein in relation to the SCM
The external jugular vein is superficial to the SCM and the internal jugular vein is underneath.

What branches does the subclavian artery give off?
The vertebral, internal thoracic and thyrocervical arteries all arise from the subclavian artery in the base of the neck.
The thyrocervical trunk gives off branches to supply the scapular region and the inferior thyroid artery (which is posterior to the common carotid artery).

Describe vertebral and internal carotid arteries
[*] Vertebral arteries arise from the subclavian arteries on left & right and ascend in the neck through transverse foramina in cervical vertebrae 6-1. They do not give off any branches in the neck.
[*] The vertebral arteries converge to form basilar artery.
[*] The internal carotid artery gives no branches off in the neck – enters skull through carotid foramen to form the Circle of Willis which is a circulatory anastomosis which also contains the basilar artery
Describe the layout of the contents of the carotid sheath
The carotid sheath is a fascial envelope of areolar tissue enclosing as well as separating the carotid artery, internal jugular vein and vagus nerve from each other. Deep cervical lymph nodes are also found within the carotid sheath. It is found deep to the sternocleidomastoid muscle and is derived from fusion of
- The prevertebral layer of cervical fascia (posteriorly)
- The pretracheal layer (anteromedially)
- The superficial layer of cervical fascia (anterolaterally)
[*] The sheath is thin over the vein but thicker around the artery.
[*] The common carotid artery lies medially within the sheath whilst the internal jugular vein is lateral (mostly under the SCM) and the nerve behind and in between the vessels.
[*] The sympathetic trunk lies outside of the sheath, medially and behind it.

Describe the clinical significance of the Carotid Triangle
[*] Boundaries
- Superior boundary – posterior belly of digastric
- Lateral boundary – anterior border of sternocleidomastoid
- Medial boundary – superior belly of omohyoid
[*] Content
- Internal jugular vein
- Bifurcation of common carotid artery
[*] Important for surgical approach to the carotid arteries or internal jugular vein
[*] Can also access vagus and hypoglossal nerves via carotid triangle.
[*] Carotid pulse can be felt in carotid triangle, but may also be palpated more inferiorly by pressing against SCM
[*] Carotid sinus massage: may be possible to slow HR down in some patients with supraventricular tachycardia by stimulating increase in BP by activating baroreceptors through massage.

Describe the course of the common carotid artery
- The right common carotid artery originates from bifurcation of the brachiocephalic artery behind the right sternoclavicular joint, whilst the left common carotid takes root directly from the arch of the aorta. Consequently, the left common carotid artery is slightly longer as it courses for about 2cm in the superior mediastinum before entering the neck.
- The carotids terminate midway between the angle of the mandible and the mastoid process of the temporal bone, with the upper (superior) border of the thyroid cartilage serving as a reliable anatomical landmark for this.
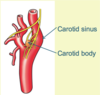
[*] Here, the carotids dilate (swells) (giving rise to the carotid sinus) as they bifurcate into almost equally bored internal and external carotid arteries. Baroreceptors are located here within the carotid sinus for detecting changes in arterial blood pressure. Peripheral chemoreceptors which detect arterial O2 are located in the Carotid Body here.
[*] The course of the common carotid artery, also known as the “carotid line” thus, is defined by a line beginning below the sternoclavicular joint and terminating midway between the angle of the mandible and the mastoid process of the temporal bone.
[*] The site of bifurcation of the common carotids (i.e. the carotid sinus) is clinically important because it can be used to alleviate supra-ventricular tachycardia through gentle rubbing (i.e. carotid massage).
Explain about a carotid artery atheroma
[*] Bifurcation of the carotid artery is a common site for atheroma formation due to turbulent blood flow => causes narrowing (stenosis) of the internal carotid artery (bruit may be heard due to the turbulence) and limiting blood flow to the brain.
[*] Rupture of the clot can cause an embolus to travel to brain via the internal carotid artery => TIA or stroke
Describe the branches of the common carotid artery
The common carotids have no collateral branches apart from terminal branching at the level of the carotid sinus.
[*] The internal carotid artery is distinguished by lack of branches in the neck as it ascends to supply intra-cranial structures.
[*] In contrast, the external carotid artery, being the major source of blood supply to extra-cranial structures of the head and neck region, gives rise to 8 branches:
- Six branches before terminating: superior thyroid, lingual, facial, ascending pharyngeal, occipital, posterior auricular
- Terminal branches: superficial temporal and maxillary
[*] The external carotid artery divides into the maxillary and superficial temporal arteries at a level behind the neck of the mandible, within the parotid gland. Here it is accompanied by the facial nerve and the retromandibular vein.

Describe the blood supply to the scalp
[*] Vessels of the scalp lie in the subcutaneous connective tissue layer.
[*] Rich blood supply with many anastomoses
[*] Largely branches of the external carotid artery (superficial temporal, posterior auricular and occipital) except supratrochlear and supraorbital arteries (branches of the ophthalmic artery) which arises from the internal carotid artery.

State the layers of the Scalp and explain the clinical relevance of the arterial supply to the scalp
Scalp Layers
- Skin
- Connective tissue (dense)
- Aponeurosis
- Loose connective tissue
- Periosteum
[*] Clinical Relevance
- Walls of arteries closely attached to connective tissue, limits constriction – can get profuse bleeding (tissues tend to keep arteries open)
- Numerous anastomoses – profuse bleeding
- Deep lacerations involving epicranial aponeurosis cause profuse bleeding because of the opposing pull of occipitofrontalis
- Note: blood supply to skull is mostly by the middle meningeal artery – loss of scalp doe not lead to bone necrosis

Describe the venous drainage of the scalp
Superficial veins generally accompany arteries
- Superficial temporal veins
- Occipital veins
- Posterior auricular veins
- Supraorbital and supratrochlear veins unite at medial angle of eye to form angular vein which drains into the facial vein
- Some deep parts of scalp in temporal region have veins which drain into the pterygoid venous plexus
[*] Connection between venous drainage of scalp and dural venous sinuses
- Veins of scalp connect to diploic veins of skull through several emissary veins and thus to dural venous sinuses
- Emissary veins are valveless (blood can flow in either direction)
- Infection from scalp can spread to the cranial cavity and affect meninges

Describe the blood supply to the dura and the skull + the clinical relevance
Dura: membrane covering the brain. Dura is a double layer and outermost layer (periosteal layer) is attached to the skull
[*] Rupture of the middle meningeal artery (branch of the external carotid artery):
- Middle meningeal artery supplies skull and dura.
- Fracture of skull at pterion can rupture MMA leading to an extradural haemorrhage (outside the dura). The pressure of blood collecting pulls the periosteal layer away from the inner surface of the skull.
[*] Craniotomy: to gain access to cranial cavity
Bone and scalp flap reflected inferiorly to preserve blood supply during treatment of rupture of the MMA.

Describe the superficial arteries of the face
All arise from the external carotid except the supra-orbital and supratrochlear which are from internal carotid artery (via ophthalmic).
Facial artery pulse can be felt at inferior border of mandible, anterior to the masseter muscle.

What are the branches of the maxillary artery?
Many branches supplying muscles and deeper structures in face

Describe dural venous sinuses and venous drainage of the face
Dural Venous Sinuses
[*] Endothelium-lined spaces between periosteal and meningeal layers of dura (one layer attached to skull, one layer attached to brain)
[*] Form at dural septae
[*] Receive blood from large veins draining brain.
[*] The sigmoid sinuses continue as the internal jugular veins, leaving the skull through the jugular foramina
Venous Drainage of the face: the supraorbital, supratrochlear, angular, superior and inferior labial veins all drain into the facial vein which drains into the common facial vein which drains into the internal jugular vein.

Describe Cavernous Sinus and connections between facial vein, cavernous sinus and pterygoid venous plexus
Cavernous Sinus
[*] Plexus of extremely thin-walled veins on upper surface of sphenoid (on either side of pituitary gland)
[*] Contents
- Internal carotid artery
- CNIII oculomotor
- CNIV trochlear
- CNVI abducent
- 2 branches of trigeminal – CNV1 ophthalmic and CNV2 maxillary
[*] Connection of facial veins with cavernous sinus and pterygoid venous plexus - the pterygoid venous plexus communicates with the cavernous sinus via various foramen such as foramen lacerum and foramen ovale so infection of the superficial face may spread to the cavernous sinus, causing cavernous sinus thrombosis.
- Veins of the face are valveless
- At medial angle of eye facial vein communicates with superior ophthalmic – drains into cavernous sinus
- Deep facial veins drain into pterygoid venous plexus
- Infection from facial vein can spread to dural venous sinuses
- Thrombophlebitis of facial vein – infected clot can travel to intracranial venous system

Describe the Lymphatic System including where it is absent
The lymphatic system is a system of vessels and lymphoid organs that drain tissue fluid from the extracellular compartment to the circulatory (venous) system where it originates.
[*] It is absent in the CNS, eyeball, inner ear, cartilage and bone and avascular planes (structures without a blood supply do not have a lymphatic supply)
Describe the properties of tissue fluid and the functional importance of the lymphatic system
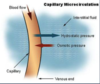
Properties of tissue fluid (aka interstitial fluid)
[*] Tissue fluid lies outside of the circulatory system and occupies the extracellular compartment of the body.
[*] It bathes all cells of the body therefore it is the widest distributed tissue in the body
[*] Its movement is not driven by a dedicated pump
- Therefore a low pressure system
- Driven by breathing and muscle contraction
[*] It is usually implicated when things start going wrong with the circulatory system, especially when cells start leaking - when lymph leave the circulatory system => oedema “collection of lymph”
Functional importance of the Lymphatic System
[*] Assists capillaries in the return of plasma proteins that leak into extracellular space
[*] Assists in the transport of cellular debris that does not use the circulatory system
[*] Essential for immunological functions of the body
[*] It absorbs/transports fats from the digestive system
[*] Plays a major role in fluid balance of the body
[*] It plays a major part in the determination of cell volume
Describe the clinical importance of the lymphatic system
[*] Major constituent of the immune system
[*] Conduit for the spread of infections, malignancies diseases (site for secondary tumours) and also be a site for primary tumours
[*] Blockage of the lymphatic system leads to lymphoedema.
[*] It is a primary site for infections
What is Lymph? How is it formed? Describe the composition of lymph
Lymph
[*] It’s a transudative fluid, aka interstitial fluid
[*] Transparent and yellowish in appearance (can depend on location within body)
[*] Alkaline in nature
Lymph is formed when the watery phase of blood leaves capillaries of the circulatory system, passing into the extracellular compartment
[*] 9/10 of the blood volume passing through tissues returns via the venous system.
[*] 1/10 of the blood volume passing through tissues returns via the lymphatic system
[*] This slight imbalance creates lymph
[*] “Chyle” is lymph produced by the small intestines.
Composition of Lymph
[*] It is composed from water as a solvent and solutes.
[*] Water makes up 96% of volume of lymph.
[*] Solutes make up 4% of volume of lymph
- Proteins: 2-6%
- Lipids: 5-15%
- Carbohydrates – mainly glucose – 132mg/100ml
- Electrolytes: sodium, calcium, potassium, chloride and bicarbonate
- Cells: mainly lymphocytes – 1000 to 2000 ml-3
[*] At rest the body produces around ~1.5-3/4 litres of lymph per day
[*] At rest it is estimated that lymph flows at a rate of 120ml/hour
- 100ml flow through the thoracic duct
- 20ml flow through the right lymphatic duct
Describe the constituents of the lymphatic system and distribution of lymph nodes in the body
[*] Wide network of lymph channels: microscopic ‘blind’ lymphatic capillaries coalesce to produce larger lymphatic vessels (or lymphangions) => collecting trunks => unite to form ducts
[*] Lymph organs: bone marrow, spleen, thymus gland, lymph nodes, tonsils
[*] Subclavian vein on both sides is the terminal part where the lymph re-join the circulatory system
Distribution of Lymph Nodes In the Body:
[*] A normal young adult body has 400-450 lymph nodes
[*] It is generally held that 2/3 of all the body’s lymph nodes are found in the abdomen
- Head & Neck - 60-70
- Arms and superficial thorax – 40
- Legs (including superficial buttocks) – 30
- Thorax – 100
- Abdomen and pelvis - 230

Describe the structure of a lymph node
[*] Kidney or bean-shaped
[*] Variable in size (up to 2.5cm in diameter) – can be dependent on location
[*] They are inhabited by phagocytes and macrophages that clean up lymph
[*] Lymph enters through afferent channels, percolates through the sinuses and leaves through the efferent channel; lymph nodes act as a filter for the fluid – remove lymph and other debris.
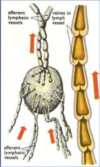
Describe the histology of a lymph node
- The region of the lymph node cortex deep to the follicles is known as the paracortex. The main type of cell that occupies the paracortex is the T-lymphocytes
- Blood vessels and efferent lymph vessels connect to the lymph node at the hilus (indicated by the circle).

Describe the general organisation of drainage of lymph
[*] Lymph in superficial structures (such as skin) drains differently from lymph in deep structures (such as visceral organs). There are therefore 2 separate drainage systems: drainage of lymph in superficial structures and drainage of lymph in deep structures.
[*] Superficial lymph vessels drain the skin and follow venous drainage.
[*] Superficial lymph vessels always drain into deep lymph vessels.
[*] Deep lymph vessels tend to accompany arteries.
[*] Exception: deep lymph nodes of the head and neck tend to follow veins.
[*] Lymph drains from superficial lymph channels to deep lymph channels. Superficial and deep lymph channels drain into lymph nodes along their courses.
- Lymphatic channels start as blind microscopic channels, gradually becoming vessels.
- Large lymphatic trunks unite to form either the right lymphatic duct or the thoracic duct.
- Lymph ducts drain into the venous system, returning it into the circulatory system – ducts drain into the subclavian vein.
Within the circulatory system, lymph becomes a constituent of blood.
[*] There are 2 lymphatics ducts separated by the midline. These ducts are vulnerable in trauma injuries e.g. stabbings.
- Right lymphatic duct (located on the right side)
- Thoracic duct (located on the left side)