SM 198a - Calcium and Phosphate Flashcards
(45 cards)
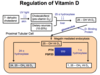
FGF-23 will ___________ production of 1,25-OH2 Vitamin D3 (active) by [stimulating/inhibiting] __________________.
FGF-23 will decrease production of 1,25-OH2 Vitamin D3 (active) by inhibiting 25 alpha hydroxylase .
FGF-23 is secreted in response to too much serum phosphorous
What belongs in box E?

1,25-OH2-D3
The active form of vitamin D3
PTH upregulates 1 alpha hydroxylase activity -> more 1,25-OH2-D3 -> works to increase serum Ca2+
FGF23 inhibits 1 alpha hydroxylase activity -> less 1,25-OH2-D3 -> works to decrease serum Ca2+

Which 3 enzymes are important for the synthesis of active vitamin D?
- 25 alpha hydroxylase (liver)
- Cholecalciferol -> 25-OH-D3
- 24 alpha hydroxylase (renal PCT cell)
- 25-OH-D3 -> inactive 24,25-OH2-D3
- 25 alpha hydroxylase (renal PCT cell)
- 25-OH-D3 -> active 1,25-OH2-D3
Also: UV light to convert 7-dehydrocholesterol to cholecalciferol

What is the effect of PTH on Ca2+ reabsorption in the intsetine?
PTH has no direct effect on Ca2+ reabsorption in the intestine
Vitamin D (1,25 Hydroxy-D3) is the primary regulator of Ca2+ reabsorption in the intestine
However, PTH secreted in response to low Ca2+ increases activation of vitamin D in the kidney, thus indirectly increaseing Ca2+ reabsorption in the intestine
How does FGF-23 affect phosphorous homeostasis?
FGF-23 promotes the excretion of phosphorous to lower serum phosphorous levels

What factors regulate PTH secretion from the chief cells of the parathyroid gland?
- Promote PTH synthesis and release
- Low Ca2+ levels
- Inhibit PTH synthesis and release
- High Ca2+ levels
- High vitamin D
- FGF-23
- Phosphorous

What is the effect of gastric acid on Ca2+ reabsorption?
Gastric acid enhances Ca2+ absorption
Low PTH is a physiological response to ____________
Low PTH is a physiological response to high Ca2+
Describe Ca2+ reabsorption in the thick ascending limb of the loop of Henle
- K+/Na+/2Cl- cotransporter (NKCC2) in the apical membrane gets these ions from the lumen to the epithelial cell
- Na+/K+ ATPase on the basolateral membrane moves Na+ into the interstitium and K+ into the epithelial cell – electrically neutral
- Chloride channels on the basolateral membrane transport Cl- ions are into the insterstitium
- ROMK on the apical membrane pumps K+ back into the lumen -> positive charge in the lumen
- This positive charge drives paracellular Ca2+ reabsorption through claudin 16

What is the most common cause of hypocalcemia?
Low PTH
- Usually post-surgical
- Thyroidectomy, parathyroidectomy, radial neck dissection
- Autoimmune or genetic possible
Describe the clinical manifestation of hyposphosphatemia
- Neuro
- Lethergy
- Paraesthesia
- Siezure
- Cardiac
- Arrhythima
- Hypotension
- Hematologic
- Hemolysis
- Skeletal
- Bone demineralization (to increase serum phosphate)
______ is the single most important factor that affects PTH secretion
Serum Ca2+ level is the single most important factor that affects PTH secretion
- High Serum Ca2+
- Ca2+ binds to CaSR on the chief cells of the parathyroid gland
- Inhibits PTH production and secretion
- Low Serum Ca2+
- Ca2+ does not bind to CaSR
- PTH is produced and released from the chief cells of the parathyroid gland
What stimulus promotes the secretion of FGF-23?
What is the effect?
FGF-23 is secreted in response to too much serum phosphorous
FGF-23 -> Decreased Vitamin D synthesis -> decreased phosphorous absorption from the intestine
In primary hyperparathyroidism, would you expect the following serum levels to be high or low?
Calcium:
Phosphorous:
1,25-OH2-D3:
- Calcium: High
- Increased renal reabsorption
- Increased active vitamin D -> increased intestinal reabsorption
- Increased resorption from bone
- Phosphorous: Low
- Decreased renal reabsorption
- 1,25-OH2-D3: Varies
- Increased vitamin D synthesis in the kidney, but some studies have shown that primary hyperparathyroidism is associated with vitamin D deficiency
What is the role of CaSR on Ca2+ reabsorption in the distal convoluted tuble?
In the DCT, CaSR is located on the apical membrane
- CaSR senses increased Ca2+ in the urine
- If Ca2+ in the urine is high, CaSR stimulates increased reabsorption of PO4 to prevent kidney stone formation

What factors affect GI absorption of calcium?
- Increase absorption
-
Vitamin D (1,25-OH2-D3)
- PTH indirectly, by increasing Vitamin D syntheisis
- Gastric acid
-
Vitamin D (1,25-OH2-D3)
- Decrease abosrption
-
Billiary and pancratic insufficiency
- Ca2+ binds to unabsorbed fat and is excreted
-
Serum hypercalcemia
- Via CaSR, which binds to Ca2+ and inhibits the effects of vitamin D
-
Billiary and pancratic insufficiency
What is the effect of PTH on reabsorption of Ca2+ in the kidney?
PTH is secreted when Ca2+ is low, and workds to increase reabsorption of Ca2+ in the thick ascending limb of the loop of Henle
- PTH increases Claudin 16 production
- Ca2+ must pass through Claudin 16 in order to be reabsobed paracellularly in the thick ascending limb

Describe the process of intestinal absorption of phosphorous
Transcellular transport:
-
NaPi-IIb: Lumen -> intestinal cell
Absorbs HPO4- with 2 Na+ - Unknown channel: Intestinal cell -> interstitium
There is also a paracellular pathway

What substance regulates Calcium absoprtion in the intestine?
1,25 Hydroxy-D3 (The active form of vitamin D)
- If Ca2+ levels are high, Ca2+ binds to the Ca2+ sensing receptor (CaSR)
- CaSR downregulates 1,25 Hydroxy-D3 synthesis
- Decreased 1,25 Hydroxy-D3 -> decreased Ca2+ absorption
- If Ca2+ levels are low, CaSR does not downregulate 1,25 Hydroxy-D3 synthesis
- The presence of 1,25 Hydroxy-D3 -> Ca2+ absorption
What is the effect of CaSR activation on the epithelial cells of the thick ascending loop?
CaSR binds to Ca2+ when serum Ca2+ levels are elevated
Binding of Ca2+ to CaSR downregulates Ca2+ reabsorption:
- Decreased ROMK activity
- -> Decreased liminal positivity
- -> Decreased driving force for Ca2+ reabsorption
- Decreased Claudin 16 production
- -> Fewer channels for paracellular Ca2+ reabsorption in the thick ascending limb of the loop of Henle

Describe the clinical manifestation of hyperphosphatemia
- Symptoms of hypocalcemia
- Phosphorous binds to Ca2+, thus reducing the amount of ionized Ca2+
- Bone fractures, stomach cramps, dysrhythmia, irritability, anxiety, carpopedal spasm, siezure
- Itching
- Metastatic calcifications
What are the expected levels for a patient with hyperparathyroidism?
Calcium:
Phosphorous:
Calcium: high
Phosphorous: low
PTH = increased renal Ca2+ reabsorption and phosphorous excretion
Describe the process of phosphorous reabsorption in the renal tubules
- NaPi-IIa and NaPi-IIc: Lumen -> Tubular epithelial cell
- Unknown channel: Tubular epithelial cell -> interstitium

What factors regulate phosphorous reabsorption in the renal tubules?
-
FGF-23
- Acts on FGFR-1 and Klotho to promote the excretion of phosphorous
-
PTH
- Promotes the excretion of phosphorous by preventing reabsorption