Spine (2008-2019) Flashcards
(38 cards)
- 4 features of Brown-Sequard Syndrome (2010, 2012)
- Ipsilateral voluntary motor loss
- Unilateral UMN findings
- Ipsilateral vibration loss
- Contra-lateral pain/temperature loss
- List 3 features of central cord syndrome. (2011, 2014)
JAAOS 2009 - Central Cord
- Upper extremities are more severely affected than lower
- Distal more than Proximal
- Sacral Sparing
- Bowel and bladder only in severe cases
- List 3 factors that would help you diagnose an incomplete spinal cord injury? (2015)
JAAOS - Thoracolumbar Spine Trauma: I. Evaluation and Classification
- Sensory function below the level of the injury
- Voluntary motor control below the level of the injury
- Sacral Sparing
- List 3 examination features suggestive of sacral sparing. (2013)
From ASIA worksheet:
- Presence of intact perianal sensation (light touch and pin prick)
- Presence of voluntary anal sphincter contraction
- Presence of deep anal sensation (to deep pressure) on digital rectal exam
- Formula for pelvic incidence (2012)
- Pelvic incidence = pelvic tilt + sacral slope
- ASIA score question. List the 11 myotomes and corresponding muscle groups. (Variations - 2011, 2012, 2013, 2014, 2016)

- 3 ways to do posterior C1-2 fusion (2012)
- Trans-articular Screws (Magerl)
- Sub-laminar wires
- Lateral Mass Screw Fixation
- What are two important considerations to take into account for placing C1-C2 trans-articular screws. (2011)
JAAOS - Posterior fixation of the cervical spine
- Location of vertebral artery
- Avoid Bicortical Screws because:
- Location of internal carotid (anteromedial)
- Hypoglossal nerve
- Limitations in head position/body habitus
- Maintain reduction, severe thoracic kyphosis, ability to get trajectory
- Hypoplastic C2 pars (variable individual anatomy)
- Reducible C1-C2 articulation
- List 3 spine conditions that enhance with gadolinium enhanced MRI (2012, 2013, 2014)
JAAOS - MRI in the Spine
- Scar tissue enhances (including granulation tissue, i.e. TB)
- Infection
- Tumors
- ** Chronic disks are dark.
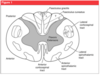
Rubrospinal tracts in the spinal cord carry: (these were long answers; look up your spinal cord anatomy.)
- Autonomic
- Voluntary Motor Control – corticospinal tract
- Flexor Muscles - rubrospinal
- Loss of muscle tone and involuntary muscle movements. - spinocerebellar
- Sexual Function - autonomic
ANSWER: C
2013

11.All of the following regarding spinal tracts true except:
- Anterior corticospinal tracts carry less motor than lateral corticospinal tracts
- Lateral corticospinal tracts are called pyramidal tracts
- Lateral corticospinal tracts arranged so that cervical spine is more central than sacral spine
- Posterior sensation tracts arranged so that the cervical spine ascending tracts are more central than sacral spine
ANSWER: D
2010, 2013, 2015 (variants)
12.A patient sustains a gunshot wound to the right side of the neck. He develops a Brown-Sequard syndrome. Which of the following is true regarding his neurologic deficits?
- Loss of motor function to right upper and lower extremities, ipsilateral loss of pain and temperature
- Loss of motor function to right upper and lower extremities, contralateral loss of vibration and position sense
- Loss of motor function to right upper and lower extremities, contralateral loss of pain and temperature sensation
- Loss of motor function to right upper and lower extremities, contralateral loss of pain and vibration
ANSWER: C
2014, 2015
13.Given a sagittal MRI showing cervical stenosis and myelomalacia. Patient had fall and presents with neck pain. No neuro deficits described. What is the most likely physical exam finding
- UE > LE weakness, distal > proximal
- LE > UE weakness, distal > proximal
- UE > LE weakness, proximal > distal
- LE > UE weakness, proximal > distal
ANSWER: A
2008, 2015
JAAOS 2009 - Central Cord Syndrome
- Upper extremities affected more than lower extremities
- Hands most affected
- Urinary retention, bowel and sexual dysfunction in most severe cases
14.Injury to what causes of retrograde ejaculation
- Inferior hypergastic plexus
- Superior hypogastric plexus
- Inferior hypogastric plexus
- Superior hypergastric plexus
ANSWER - B
2009, 2013, 2014
Retrograde Ejaculation After Anterior Lumbar Interbody Fusion: Transperitoneal Versus Retroperitoneal Exposure. Sasso, Burkus and LeHuec. Spine. 2003
- Damage to the superior hypogastric plexus during exposure of the anterior lumbosacral spine can denervate this bladder neck sphincter, resulting in retrograde ejaculation.
15.Regarding anterior approach to T-spine, which is false?
- Aorta blocks visualization of high to mid-T-spine on left
- liver blocks visualization of lower T-spine on right
- Resect T11 rib head to access T11-12 disc space – rib head 11 = T10/11
- Resect a rib 1-2 levels above the area of interest during approach
ANSWER - C
2010, 2014
- Anterior Transthoracic thoracic spine approach– resect rib 2 levels above (see pic)
- Anterior Transabdominal thoracic spine – resent T10 rib for approach
- Combo AO, JAAOS, hoppenfelds
- Right sided for T2-T9 (aorta and heart on left)
- Left sided for T10-L2 avoids liver on right
16.Regarding the anterior approach to the cervical spine, all of the following are true EXCEPT?
- Omohyoid transection improves access to the lower C spine
- The parasympathetic trunk is at risk
- Sub-platysmal fascial dissection improves exposure
- The recurrent laryngeal nerve runs in the tracheoesophageal groove
ANSWER - B
2014
- OKU Spine 4
- Course of recurrent laryngeal nerve
- Branch of the vagus nerve
- Right –> arises anterior to subclavian artery, curves behing it, ascends to side of trachea
- Left –> loops under arch of aorta
- At C7 the nerve lies deep within the esophagotracheal groove on the left, but anterior and lateral to it on the right
- Operative Techniques - Anterior approach to the cervical spine (p4507-4510)
- “blunt dissection with scissors undermines the edges of the platysma
- Allows for greater mobilization of the soft tissues, which is helpful in accessing the multiple disc levels
- Dividing the omohyoid will allow for a more extensile cephalad-cuadal exposures and less tehnsion on the wound for easier placement of plates and screws
17.Contents of the carotid sheath include the carotid artery, internal jugular vein, and what other structure?
- Vagus nerve
- phrenic nerve
- Vagus and phrenic nerve
- Vagus and sympathetic
ANSWER: A
2011
Hoppenfeld:
- The carotid sheath enclosing the common carotid artery, vein and vagus nerve can now be exposed
18.How do you calculate the Power’s ratio where B=basion, A=anterior arch of atlas, O=opisthion, C=posterior arch of atlas
- BA/CO
- BC/AO
- AC/BO
- AB/CO
ANSWER: B
2013, 2016

- Can do PLIF/TLIF in all of the following except
- Pseudoarthoris
- Spondylolisthesis
- Infection
ANSWER: C
2012
JAAOS 2008 - Posterior Lumbar Interbody Fusion

- All of the following associations are right except? REPEAT
- Foot Dorsiflexion - L4
- Sensation over patella L2
- Hamstring reflex L5-S1
- Hip abductors – L5
ANSWER: B
2012
- L3 provides sensation over patella
- Which of the following is associated with an increased risk of complications with halo treatment?
- Re-tightening the screws at an appropriate interval
- Placing the ring 2cm above the pinna
- Placing the ring closer to the skull
- Using 6 pins instead of 4
ANSWER: B
2011, 2014
JAAOS - The Halo Fixator
- More lateral pin insertion risks penetration of the thin temporal bone.
- More medial positioning risks injury to the supraorbital and supra- trochlear nerves.
- Spinal Associations; all of the following are true except
- Isthmic Spondylolisthesis and spina bifida occulta
- Isthmic Spondylolisthesis and pars abnormality
- Folate and Neural Tube defects (worded exactly like this)
- Degenerative spondylolisthesis and spondylosis
Answer: D
Miller’s 8th edition:
- A: Spina bifida occulta, thoracic hyperkyphosis and cheuermann disease have been associated with spondylolisthesis
- B: basically the definition of isthmic spondy
- Neural tube defect dx in utero with increased level of alpha-fetoprotein
- Related to folate deficiency in utero
- With regards to proteoglycans, all of the following are true except
- Proteoglycans are hydrophilic
- Proteoglycans are hydrophobic
- Proteoglycans are sulfated
- Proteoglycans are bound to a protein core
ANSWER: B
2012
AAOS Core Review 2:
- Proteoglycans can trap water in the ECM by their negative charge, regulating matrix hydration
- During the posterior approach to the spine, the thecal sac can be retracted?
- Above the level of the conus
- Below the level of the conus
- Below T12
- Never
ANSWER: B
2014




