Spine (Updated) Flashcards
(236 cards)
What is the ASIA spinal cord injury scale?
Asia A: Complete
- No motor or sensory function preserved in sacral elements
Asia B: Incomplete
- Sensory but not motor function preserved below neurological level
Asia C: Incomplete
- Greater than half the muscles below affected level are < antigravity power (<3/5)
Asia D: Incomplete
- Greater than half the muscles below affected level are > antigravity (>3/5)
Asia E: Normal

What are the clinical features of an upper motor neuron vs lower motor neuron lesion?

what is spinal shock
- temporary loss of motor (flaccid paralysis), sensation and reflexes as a result of an acute spinal cord injury
- state of complete areflexia as demonstrated by loss of bulbocavernosus reflex secondary to an acute spinal cord injury
- the significance is that thee extent of the neurologic injury cannot be determined until the spinal shock has resolved
- spinal shock is resolved upon return of the bulbovacernosus reflex
- usually resolves within 24h from time of injury
- bulbocavernosus test = clinical test to assess the integrity of the intact S3-S4 arc, performed by squeezing the glans penis, placing pressure on the clitoris, or tugging on a foley catheter
- an intact reflex will result in contraction of the anal sphincter
what is neurogenic shock
- hypotension and bradycardia 2° to loss of sympathetic tone as a result of an acute spinal cord injury
- typically occurs with an acute spinal cord injury above the level of T6
How do you determine the ASIA classification in a spinal cord injury?
- Determine if patient is in spinal shock
* Check bulbocavernosus reflex - Determine neurologic level of injury
- Lowest segment with intact sensation and antigravity (3 or more) muscle function strength
- In regions where there is no myotome to test, the motor level is presumed to be the same as the sensory level
- Determine whether the injury is COMPLETE or INCOMPLETE
- COMPLETE defined as: (ASIA A)
- No voluntary anal contraction (sacral sparing) AND
- 0/5 distal motor AND
- 0/2 distal sensory scores (no perianal sensation) AND
- bulbocavernosus reflex present (patient not in spinal shock)
- INCOMPLETE defined as:
- Voluntary anal contraction (sacral sparing) OR
- Sacral sparing critical to determine complete vs. incomplete
- Palpable or visible muscle contraction below injury level OR
- Perianal sensation present
- Voluntary anal contraction (sacral sparing) OR

Definition of an incomplete spinal cord injury
some preservation of sensory and/or motor function below the lesion
what are the incomplete spinal cord syndrome
- central cord syndrome
- brown-sequard syndrome
- anterior cord syndrome
- posterior cord syndrome
- connus medullaris syndrome
- cauda equina syndrome (CES)
what is the most common incomplete cord syndrome
central cord syndrome
what is the clinical presentation of central cord syndrome
- classically
- motor more affected than sensory function
- upper extremity more affected than lower extremity
- distal more than proximal
- hands and forearms most affected
- bladder (urinary retention), bowel and sexual dysfunction in severe cases
- sacral sparing
what are the clinical scenarios/presentations for complete cord syndromes
- older patient (>60), underlying cervical spondylosis, hyperextension injury, no evidence of bony spine injury
- younger patient, no underlying cervical spondylosis, high-energy mechanism, associated fractures and/or dislocations
- younger patient with congenital stenosis, hyperextension injury
- young patient with traumatic disc herniation, no spinal fracture or dislocation
what is the order of neurologic recovery in complete cord syndrome?
- lower extremities → bowel/bladder control → upper extremity → hand
- motor recovery occurs caudal to cephalad (toe flexors are first to return)
- recovery is usually less complete in upper extremities compared to lower extremities
- hand recovery is variable (most common long term disability)
what is the management of central cord syndrome
- medical management
- ICU monitoring
- adequate BP (MAP >85mmHg)
- hard cervical collar
- use for at least 6 weeks or until neck pain has resolved and associated neurological improvement is noted
- early mobilization
- surgery
- absolute indication = spinal instability
- defined as angular displacement >11° or vertebral body translation >3.5mm
- early surgery is recommended in what 2 cases
- overt spinal isntability with acute dislocation
- progressive neurological deficit
- absolute indication = spinal instability
what is the clinical presentation of brown-sequard syndrome
- ipsilateral loss of all sensory modalities at the level of the lesion
- ipsilateral flaccid paralysis at the lecel of the lesion
- ipsilateral spastic paraparesis below the lesion
- ipsilateral loss of vibration and position sense below the lesion
- contralateral loss of pain and temperature below the lesion
what is the clinical presentation of anterior cord syndrome
- loss of pain, temperature, crude touch sensations below the level of the lesion
- loss of motor below the level of the lesion
- orthostatic hypotension, bladder and/or bowel incontinence and sexual dysfunction
- preservation of fine touch, proprioception and vibration
clinical presentation of posterior cord syndrome
- loss of fine-touch, proprioception and vibration below the level of the lesion
- preservation of motor, pain, temperature, crude touch
what is the clinical presentation of conus medullaris syndrome
- lower extremity weakness (mixed UMN and LMN deficits)
- main difference between cauda equina syndrome (only LMN deficits)
- saddle anesthesia
- bowel and bladder dysfunction
- impotence
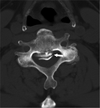
What cervical spine radiographic parameters should be assessed on plain film xrays?
- Occipitocervical junction
- Harris rule of 12
- Basion-dens interval or basion-posterior axial interval >12 suggests occipitocervical dissociation
- Power’s ratio
- Powers ratio = C-D/A-B
- C-D: distance from basion to posterior arch
- A-B: distance from anterior arch to opisthion
- Ratio ~ 1 is normal
- If > 1.0 concern for anterior dislocation
- Ratio < 1.0 raises concern for:
- Powers ratio = C-D/A-B
- Posterior atlanto-occipital dislocation
- Odontoid fractures
- Ring of atlas fractures
- Atlantoaxial junction
- ADI
- > 3.5mm considered unstable
- > 10mm indicates surgery in RA
- PADI/SAC
- <14mm indicates surgery in RA
- Lateral ADI
- 1-2mm of asymmetry of lateral mass alignment relative to dens may be normal
- Combined lateral mass overhang
- >8.1mm indicates transverse ligament rupture and unstable injury
- Subaxial spine
- >8.1mm indicates transverse ligament rupture and unstable injury
- Anterior vertebral line
- Posterior vertebral line
- Spinolaminar line
- Prevertebral soft tissue shadow
- >6mm at C2, >22mm at C6 = abnormal
- Interspinous distance
- Stacked parallelogram facets

What is the classification of occipital condyle fractures?
Anderson and Montesano Classification
- Type I - comminuted (3%)
- MOI = axial load
- Stable injury
- Type II - basilar skull fracture extending into the occipital condyle (22%)
- MOI = shear injury
- Stable injury
- Type III - transverse avulsion fracture (75%)
- MOI = forced rotation with lateral bending (alar ligament avulsion)
- Potentially unstable (associated with craniocervical dissociation)

What cranial nerve palsies may develop in association of occipital condyle fractures?
CN IX, X, XI
- travel in jugular foramen adjacent to occipital condyle
What is the management of occipital condyle fractures?
- Type I and II = external immobilization (cervical orthosis)
- Type III = depends on if associated with craniocervical dissociation or ligamentous instability
- Stable = external immobilization (cervical orthosis)
- Unstable = occipitocervical fusion
- C0-C2(or C3) instrumentation and fusion

What are the two main presentations of occipitocervical instability?
[Orthobullets]
- Traumatic – often fatal
- Acquired – often associated with Down’s syndrome
What are the radiographic parameters to be assessed on plain film for craniocervical dissociation?
[JAAOS 2014;22:718-729]
- Harris lines (Harris rule of 12s)
- Basion-dens interval
- Normal = <12mm
- Distance from basion to tip of dens
- Basion-axis interval
- Normal = 4-12mm
- Distance between line parallel to posterior cortex of C2 and basion
- Powers ratio [Orthobullets]
- Distance from basion to posterior arch C1/distance from opisthion to anterior arch C1
- Normal = 1
- >1 = anterior dislocation
- <1 = posterior dislocation, dens fracture, ring of atlas fracture
- Wackenheim line
- Line parallel along the posterior portion of the clivus to the upper cervical spine
- Normal = tip of dens is <1-2mm from Wackenheim line

What is the classification system for occipitocervical instability based on direction of displacement?
[Orthobullets]
Traynelis Classification
- Type 1 - Anterior occiput dislocation
- Type 2 - Longitudinal dislocation
- Type 3 - Posterior occiput dislocation
What is the classification system for occipitocervical instability based on degree of instability?
[JAAOS 2014;22:718-729]
Harbourview Classification
- Stage I - minimal or nondisplaced (STABLE)
- Often unilateral injury to the craniocervical ligaments
- Treatment:
- External immobilization
- Stage II - minimally displaced (STABLE or UNSTABLE)
- MRI indicates significant soft tissue injury (does not indicate instability)
- Proceed with traction test
- Provocative traction fluoroscopy
- Technique – patient supine with lateral fluoro view centred at C1, Gardner Wells tongs are applied and 5lbs are added (repeat fluoro) then increased to 10lbs (repeat fluoro)
- Positive traction test = Fracture displacement >2mm, atlanto-occipital distraction >2mm, or atlantoaxial distraction >3 mm indicates CCJ instability
- Treatment
- Stable = external immobilization
- Unstable = occipitocervical fusion (C0-C2 or C3)
- MRI indicates significant soft tissue injury (does not indicate instability)
- Stage III – gross craniocervical misalignment
- BAI or BDI >2mm above upper limit of normal
- Usually fatal
- Treatment:
- Occipitocervical fusion (C0-C2 or C3)