Systemic Lupus Erythematosus Flashcards
(32 cards)
What is SLE?
A multisystemic autoimmune disease with inadequate T cel suppressor activity and increased B cell activity.
It is autoantibody driven where patients have antibodies to certain cell nucleus components.
There is inadequate clearance of immmune complexes resulting in a host of immune responses which cause tissue inflammation and damage.
Epidemiology of SLE.
9 times more common in women.
It is usually premenopausal women.
Peak age of onset is between 20 and 40 years.
Aetiology of SLE.
Heredity and genetics
Sex hormone status (pre-menopausal more common)
Drugs lik hydralazine, isoniazid, procainamide and penicillamine can induce a mild form of SLE.
UV light triggers flares (rash is photosensitive)
Exposure to EBV.
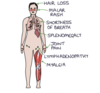
Common symptoms and signs of SLE.
Mnemonic SOAP BRAIN.
Serositis - pleurisy and pericarditis
Oral ulcers
Arthritis - small joints non-erosive
Photosensitivity - malar or discoid rash
Blood disorders
Renal involvment - GN
Autoantibody postive
Immunlogic tests
Neurologic disorder - seizures or psychosis.
Expain oral ulcers in SLE.
Usually painless.
Palate is most specific
Blood disorders in SLE.
Low WCC
Lymphopenia
Thrombocytopenia
Haemolytic anaemia
General features of SLE.
Fever is common in exacerbations
Malaise and tiredness.
Systems involved in SLE.
Joints - > 90%
Skin - 85%
Lungs - 50%
CVS - 25%
Kidneys - 30%
Nervous system - 60%
Eyes
GI
Skin features of SLE.
Photosensitivity
Butterfly rash
Vasculitis
Purpura
Urticaria
Joint features of SLE.
Aseptic necrosis of hip (rare)
Arthritis of small joints
Lung features of SLE.
Pleurisy
Pleural effusion
Restrictive lung defect with fibrosis (rare)
CVS features of SLE.
Pericarditis
Endocarditis
Aortic valve lesions
Raynaud’s
Vasculitis
Arterial and venous thromboses
Kidney features of SLE.
Lupus nephritis
Nervous system features of SLE.
Fits
Hemiplegia
Ataxia
Polyneuropathy
Cranial nerve lesions
Psychosis
Demyelinating syndromes
Eye features of SLE.
Retinal vasculitis
Episcleritis
Conjunctivitis
Optic neuritis
2ndary Sjögren’s syndrome
Investigations of SLE.
FBC
U&Es
Autoantibodies
Serum complement
Urinalysis
Skin and renal biopsy
Imaging
FBC features in SLE.
May show leucopenia, lymphopenia and/or thrombocytopenia.
Anaemia of chronic disease or autoimmune haemolytic anaemia might be present.
ESR is raised and plasma viscosity is raised however CRP is normal.
U&Es features of SLE.
Urea and creatinine only rise when renal disease is advanced.
Low serum albumin or high urine albumin:creatinine ratio are earlier indicators of lupus nephritis.
Autoantibodies suggestive of SLE.
ANAs such as;
anti-dsDNA
anti-Ro
anti-Sm
anti-La
They are present in 90% of cases.
What does antiphospholipid antibodies suggest?
Increased risk of pregnancy loss and thrombosis.
Antiphospholipid antibodies and antiphospholipid syndrome can occur secondary to SLE. They can occur in up to 40% of patients with SLE and are associated with an increased risk of venous thromboembolism.
How can anti-DsDNA be used?
Titre rises with disease activity.
C3 and C4 levels in SLE.
It will fall in active disease.
A combination of high ESR, high anti-dsDNA and low C3 may herald a flare of disease.
Diagnostic criteria of SLE.
You can use the SLICC Criteria or the ACR Criteria for establishing a diagnosis.
Any ≥4 of the 11 criteria are required to classify a patient as having SLE.
This is ACR criteria
1 - Malar rash
2 - Discoid rash
3 - Photosensitivity
4 - Oral ulcers
5 - Arthritis
6 - Serositis
7- Renal disorder
8 - Neurological disorder
9 - Haematological disorder
10 - Immunologic disorder
11 - Antinuclear antibody
Laboratory criteria of SLE.
(Based on SLICC criteria)
+ve ANA
Anti-dsDNA
Anti-Sm
Antiphospholipid Abs
Low complement
+ve Direct Coombs test


