The Kidneys in Systemic Disease Flashcards
(44 cards)
What organ receives the most blood flow per unit volume?
Kidneys
What are the different things that can happen to proteins at the glomerular?
Glomerular may filter proteins which are then reabsorbed by the tubule epithelial cells:
Or may trap proteins or immune complexes
What are some systemic diseases that affect the kidney?
- Diabetes mellitus
- CVD
- Cardiac failure
- Atheroembolism
- Hypertension
- Atherosclerosis
- Infection
- Sepsis
- Post-infectious GN
- Infective endocarditis
- Inflammation in blood vessels
- SLE
- Vasculitis
- Scleroderma and other connective tissue diseases
- Cryoglobulinaemia
- HUS/TTP
- Myeloma
- Amyloidosis
What are some drugs that affect the kidneys?
- Aminoglycosides
- ACE inhibitors
- Penicillamine, gold
- NSAIDs
- Radiocontrast
Describe the natural history of diabetic nephropathy?
- Silent sub-clinical phase
- Hyperfiltration
- Increased GFR
- Microalbuminuria (20-200ug/d)
- Clinical nephropathy (proteinuria > 0.5g/d)
- Established renal failure
So causes development of proteinuria and decline in GFR

Describe the long term risk of diabetic nephropathy with type 1 and 2 diabetes?
- Type 1 diabetes
- 4% develop nephropathy within 10 years
- 25% develop nephropathy within 25 years
- Type 2 diabetes
- 10% develop nephropathy within 5 years
- 30% develop nephropathy within 20 years
- 30% of those with diabetic nephropathy will progress to ESRF
What percentage of people with diabetic nephropathy will progress to ESRF?
30%
What is the single commonest cause of ESRF?
Diabetes
Is the incidence of ESRF due to diabetes increasing or decreasing?
Increasing
Out of type 1 and 2 diabetes, who is at the greatest risk of diabetic nephropathy?
Equal risk
What is increasing proteinuria usually associated with in terms of GFR?
Declinging GFR
What is chronic kidney disease classified based on?
Classification is based on kidney function (GFR)
What classification system does CKD use?
Uses NKF K/DOQI classification system

What is stage 1 CKD?

What is stage 2 CKD?

What is stage 3 CKD?
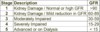
What is stage 4 CKD?

What is stage 5 CKD?

What is the relationship between CKD and CVD?

What is the commonest cause of renal failure in older patients?
Commonest cause of renal failure in older patients is reno-vascular disease:
- Atheroembolic disease
- Eosinophilia
- Peripheral skin lesion
- Warfarin therapy
- Vascular procedures
What is vasculitis?
Is inflammatory reaction in the wall of any blood vessel
What is vasculitis defined by?
Defined by size of vessels involved
Explain the nomenclature of vasculitis?
- Aorta/large artery
- Takayasu arteritis
- Giant cell arteritis
- Medium artery
- Polyarteritis nodosa
- Kawasaki disease
- Small vessel
- Wegener’s granulomatosis
- Granulomatous inflammation in respiratory tract
- Focal necrotising glomerulonephritis with crescents
- Slightly more common in males
- Affects all age groups, most common 40-60 years
- Upper respiratory tract symptoms
- Epistaxis, nasal deformity, sinusitis, deafness
- Lower respiratory tract symptoms
- Cough, dyspnoea, haemoptysis
- Pulmonary haemorrhage
- Other organs
- Kidney – glomerulonephritis
- Joints – arthralgia, myalgia
- Eyes – scleritis
- Heart – pericarditis
- Systemic – fever, weight loss, vasculitic skin rash
- Microscopic polyarteritis
- Can present with systemic disease, renal and pulmonary involvement
- More commonly renal limited disease
- Churg-Strauss syndrome
- Wegener’s granulomatosis
What is vasculitis of aorta/large artery called?
- Takayasu arteritis
- Giant cell arteritis


