Ulcerative Colitis Flashcards
(34 cards)
Who is commonly affected by ulcerative colitits (UC)?
It is most prevalent among the Caucasian population, with the presentation following a bimodal distribution between 15-25yrs for most cases and a smaller peak of incidence between 55-65yrs.
Briefly describe the course of the disease
The disease typically follows a remitting and relapsing course. A severe fulminant exacerbation may be life-threatening, resulting in severe systemic upset, toxic megacolon, colonic perforation, and even death.
What is shown in the image?

Histology of Bowel Segment in UC, showing non-granulomatous inflammation with crypt abscess (circled) formation.
Briefly describe the pathophysiology of UC
Although the exact aetiology of ulcerative colitis is unknown, current theories suggest it develops as an interaction between genetic factors and environmental triggers.
It is characterised by diffuse continual mucosal inflammation of the large bowel, beginning in the rectum and spreading proximally, potentially affecting the entire large bowel. A portion of the distal ileum can become affected in a small proportion of cases, termed ‘backwash ileitis’ (if the ileocaecal valve is not competent).
Histological changes include inflammation of the mucosa and submucosa, crypt abscesses, and goblet cell hypoplasia. Repeated cycles of ulceration and healing may lead to raised areas of inflamed tissue termed ‘pseudopolyps’.
What is the link between smoking and UC?
Smoking is protective against UC.
Briefly differentiate between UC and Crohn’s
Note: site involvement, inflammation, macroscopic changes and microscopic changes

What are the clinical features of UC?
Note: signs and symptoms
Ulcerative colitis is typically insidious in onset. The cardinal feature is bloody diarrhoea, with visible blood in stool reported in more than 90% of cases.
The most common manifestation of ulcerative colitis is proctitis, whereby the inflammation is confined to the rectum. Patients will complain of PR bleeding and mucus discharge, increased frequency, urgency of defecation, and tenesmus.
Patients presenting with more widespread colonic involvement are more likely to experience bloody diarrhoea with clinical features of dehydration and electrolyte imbalance. Systemic symptoms also include malaise, anorexia, and low-grade pyrexia.
What are the clincial features of UC?
Note: on examination
Unless there is a severe exacerbation, clinical examination is generally unremarkable.
Fulminant colitis, toxic megacolon, or colonic perforation should be suspected if the patient complains of severe abdominal pain and on examination demonstrates systemic involvement or signs of peritonism.
What is the name of the grading criteria for UC?
Truelove and Witt criteria.
Describe mild UC according to Truelove and Witt Criteria
Note: bowel movements per day, blood in stool, pyrexia, pulse, anaemia and ESR

Describe moderate UC according to Truelove and Witt Criteria
Note: bowel movements per day, blood in stool, pyrexia, pulse, anaemia and ESR

Describe severe UC according to Truelove and Witt Criteria
Note: bowel movements per day, blood in stool, pyrexia, pulse, anaemia and ESR

What other systems are affected by UC?
- MSK
- Skin
- Eyes
- Hepatobiliary
What are the extra-intestinal MSK manifestations of UC?
Enteropathic arthritis (typically affecting sacroiliac and other large joints) or nail clubbing.
What are the extra-intestinal skin manifestations of UC?
Erythema nodosum (tender red/purple subcutaneous nodules, typically found on the patient’s shins).
What are the extra-intestinal eye manifestations of UC?
Episcleritis, anterior uveitis or iritis.
What are the extra-intestinal hepatobiliary manifestations of UC?
Primary sclerosing cholangitis (chronic inflammation and fibrosis of the bile ducts).
What is shown in image A and B?

Erythema nodosum.
What investigations should be ordered for UC?
Note: laboratory
Routine bloods (FBC, U&Es, CRP, LFTs, and clotting) are required to examine for anaemia, low albumin (secondary to malabsorption), and evidence of inflammation (raised CRP and WCC).
In the UK, NICE guidelines recommend that faecal calprotectin testing is carried out in patents with recent onset lower gastrointestinal symptoms; it is raised in inflammatory bowel disease, but unchanged in irritable bowel syndrome. A stool sample should be sent for microscopy and culture.
What investigations should be ordered for UC?
Note: imaging
The definitive diagnosis for ulcerative colitis is via colonoscopy with biopsy. Characteristic macroscopic findings are of continuous inflammation with possible ulcers and pseudopolyps visible. A flexible sigmoidoscopy may be sufficient and in clinical practice full colonoscopy is only required if the diagnosis is unclear; colonoscopy should be avoided in acute severe exacerbations.
In acute exacerbations, an abdominal radiograph (AXR) or CT imaging are used to assess for toxic megacolon and/or bowel perforation has occurred. AXR features of acute ulcerative colitis flares also include mural thickening and thumbprinting, indicating a severe inflammatory process in the bowel wall; in chronic cases of UC, a lead-pipe colon is often described- but this is usually best seen on barium studies.
What is shown in image A?
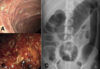
(A) bowel fibrosis, secondary to chronic UC
What is shown in image B?

(B) active inflammation in patient with UC.
What is shown in image C?

(C) AXR changes in active UC, showing toxic megacolon with lead-pipe colon (seen in descending colon).
Why should anti-motility drugs, such as loperamide, should be avoided in acute attacks?
Anti-motility drugs, such as loperamide, should be avoided in acute attacks, as these can precipitate toxic megacolon.



