✅ URI / UTI / STD / SEPSIS / TB Flashcards
(176 cards)
💨 UPPER RESPIRATORY INFECTION
Usually viral syndrome that is benign and self-limited, lasting <strong>3 to 10 days</strong>. Viruses (eg, rhinovirus, coronavirus, respiratory syncytial virus, metapneumovirus) cause infection by gaining entrance to epithelial cells of the upper respiratory tract, leading to host inflammatory responses, cholinergic stimulation, vasodilation, and increased vascular permeability.
<strong>Tx:</strong> Inhaling heated vapor, such as steam from a hot shower, may decrease nasal symptoms. Other symptomatic measures include increasing fluid intake, gargling with salt water or using saline nasal spray, sucking on throat lozenges, and ensuring adequate rest. Although these measures lack good evidence of effectiveness, they are safe and inexpensive. For relief of nasal congestion, oral decongestants (eg, pseudoephedrine) or short-term (<3 days) use of topical nasal decongestants (eg, phenylephrine) is beneficial.
<strong>Rx:</strong> In patients with rhinorrhea and sneezing, a short course of a <strong>first-generation antihistamine diphenhydramine (Benadryl) </strong>or<strong> intranasal ipratropium</strong> may be considered. In patients with a productive cough and wheezing, an <strong>inhaled β-agonist </strong>may reduce the duration of cough. Acetaminophen or an nonsteroidal anti-inflammatory drugs (eg, naproxen, ibuprofen) may be used for headache, myalgia, and malaise.
🦠 Pneumonia
A space occupying lesion without volume loss; caused by bacteria, viruses, mycoplasmae and fungi.
Ddx: Airspace filling not distinguishable radiographically: fluid (inflammatory), cells (cancer), protein (alveolar proteinosis) and blood (pulmonary hemorrhage).
Dx: The x-ray findings of pneumonia are airspace opacity, lobar consolidation, or interstitial opacities. There is usually considerable overlap.
Lobar - classically Pneumococcal pneumonia, entire lobe consolidated and air bronchograms common. Abrupt in onset, with fever, pleuritic chest pain, and purulent sputum production.
An “Air bronchogram” is a tubular outline of an airway made visible by filling of the surrounding alveoli by fluid or inflammatory exudates.
Ddx: air bronchograms: Lung consolidation (PNA), pulmonary edema, nonobstructive pulmonary atelectasis, severe interstitial disease, neoplasm, and normal expiration.
Lobular - often Staphlococcus, multifocal, patchy, sometimes without air bronchograms
Interstitial - Viral or Mycoplasma; latter starts perihilar and can become confluent and/or patchy as disease progresses, no air bronchograms. “Ground Glass” is a radiology descriptive term (used in both chest radiographs and CT imaging) to indicate that blood vessels are not obscured as would be the case in alveolar lung opacities. Both atypical bacterial and viral organisms may produce pneumonias that differ radiographically from more common bacteria such as pneumococcus. They may produce a ground glass appearance and increased interstitial markings. The CXR appearance of Pneumocystis pneumonia is typically bilateral, diffuse interstitial (“reticular”) or ground glass opacities.
Hx: “Atypical pneumonia” due to C pneumoniae or 🏒M. pneumoniae: Patients often complain of a sore throat at the beginning of the illness and a protracted course of symptoms. Physical examination is often unimpressive compared to radiograph findings and the diagnosis is often not made as the course is often indistinguishable from other lower respiratory infections.
💨Aspiration - follows gravitational flow of aspirated contents; impaired consciousness, post anesthesia, common in alcoholics, debilitated, demented patients; anaerobic (Bacteroides and Fusobacterium). In a supine patient who has aspirated, the common locations of pneumonia are the posterior segment of the upper lobe and superior segment of the lower lobe. The superior segment of the right lower lobe is the segment most likely to develop aspiration pneumonia.
Diffuse pulmonary infections - Community acquired (Mycoplasma, resolves spontaneoulsy) nosocomial immunocompromised host (bacterial, fungal, PCP)
🏥 Nosocomial by definition occur 3 days after admission. Patients in the ICU are often relatively immunocompromised secondary to their primary disease and are subject to iatrogenic factors which increase their sucseptabilty to pneumonia-causing pathogens. These include the following: endotracheal tubes, which defeat many patient defense mechanisms; medications used to reduce gastric acid, which may promote bacterial growth in the stomach; and the use of antibiotics, which may selectively encourage the growth of some pathogenic bacteria. Nosocomial pneumonias are often polymicrobial and caused by 🔮gram-negative enteric pathogens. The offending organisms often include Pseudomonas species, E-coli, Klebsiella species, and Proteus species (Pseudomonas, debilitated, mechanical vent pts, high mortality rate, patchy opacities, cavitation, ill-defined nodular).
Ventilator-associated pneumonia (VAP) is a type of nosocomial pneumonia that usually develops >48 hours after endotracheal intubation. It is most commonly caused by aerobic gram-negative bacilli (eg, Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae) and gram-positive cocci (eg, methicillin-resistant Staphylococcus aureus, Streptococcus). Patients usually have fever, purulent secretions, difficulty with ventilation (eg, increased respiratory rate, decreased tidal volume), and leukocytosis. Those with an abnormal chest x-ray (eg, alveolar infiltrates, air bronchograms, silhouetting of adjacent solid organs) require lower respiratory tract sampling (ie, tracheobronchial aspiration) for microscopic analysis (Gram stain) and culture
🌆 Community-acquired pneumonias, which usually are caused by 🏮 gram-positive species
Dx:
The radiographic appearance of pneumonia may be difficult to differentiate from atelectasis or early ARDS. Classically, pneumonia first appears as patchy opacifications or ill-defined nodules. It is often multifocal and bilateral, occurring most often in the gravity dependent areas of the lung. This feature makes it difficult to distinguish from atelectasis or pulmonary edem. E-coli and pseudomonas species can rapidly involve the entire lung. Their symmetric pattern often simulates pulmonary edema. The presence of patchy air space opacities, air bronchograms, ill-defined segmental consolidation or associated pleural effusion support the diagnosis of pneumonia. Occassionally, in gram-negative pneumonias small luciencies may be found within consolidated lung which may represent unaffected acini or areas of air trapping. This is particularly likely to occur in patients with underlying COPD. However, these must be distinguished from lucencies created by cavitation and abscess formation.
Cx: Complications of nosocomial pneumonias can have severe consequences and require immediate attention. Unlike community acquired pneumonia, pleural effusions caused by gram-negative organisms are more likely to represent empyema and therefore require drainage. Other complications of nosocomial pneumonias include lung abscess formation and bronchopleural fistulas.
In consolidative pneumonia, the alveoli become filled with inflammatory exudate, leading to marked impairment of alveolar ventilation in that portion of the lung. The result is right-to-left intrapulmonary shunting, which describes perfusion of lung tissue in the absence of alveolar ventilation, an extreme form of ventilation/perfusion (V/Q) mismatch (V≈0). A characteristic of intrapulmonary shunting is inability to correct hypoxemia with increased concentration of inspired oxygen (FiO2). Other causes of V/Q mismatch (eg, emphysema, interstitial lung disease, pulmonary embolism) allow for correction of hypoxemia with an increase in FiO2 because V > 0. In practice, increased FiO2 typically leads to some improvement in hypoxemia in patients with pneumonia because only a portion of the lung is being affected by intrapulmonary shunting.
🏇🏿 Pneumococcal Pneumonia
α-Hemolytic streptococci
🏇🏿Streptococcus Pneumonia
💪🏿PR/MDR Pneumococcal Pneumonia
Hx: Age >65 y, β-lactam therapy (in previous 3 mo), alcoholism, immunosuppression (illness, glucocorticoids), multiple medical comorbidities, exposure to a child in a day care center.
Dx: CA-MRSA or compatible sputum Gram stain
Tx: Add vancomycin or linezolid to β-lactamb plus either azithromycin or a fluoroquinolone.
Patients with bacteremic pneumococcal pneumonia should be discharged on oral amoxicillin to complete 7 days of therapy.
Organizing pneumonia
Subacute illness (4-6 wk) with fever and alveolar infiltrates (often peripheral). Diagnosis is based on biopsy (transbronchial or open lung) or characteristic clinical picture and response to glucocorticoids.
Pneumocystis pneumonia (PCP)
Clinical
- Indolent (HIV) or acute respiratory failure (immunocompromised)
- Fever, dry cough, ↓ oxygen levels
HIV infection with a low CD4 count is the biggest risk factor; however, patients taking 🌚chronic glucocorticoids (especially in combination with other immunosuppressant medications) are at significant risk.
Workup
- ↑ LDH level
- Diffuse reticular infiltrates on imaging
- Induced sputum or BAL (stain)
Treatment
- TMP-SMX
- Prednisone if ↓ oxygen levels
Prevention
- TMP-SMX
- Antiretrovirals (in HIV)
Hx: Subacute onset of dyspnea on exertion, hypoxia, nonproductive cough; diffuse interstitial infiltrates on chest radiograph
Dx: Chest x-ray usually shows bilateral interstitial infiltrates. Hypoxia out of proportion to the radiographic findings is also suggestive. Serum lactate dehydrogenase levels are frequently elevated. The diagnosis is confirmed by demonstration of the organism in sputum or bronchoalveolar lavage aspirate.
Tx: Trimethoprim-sulfamethoxazole (TMP-SMX) is the initial drug of choice for the treatment of PCP regardless of pneumonia severity. Treatment typically lasts for 21 days. Adjunctive corticosteroids have been shown to decrease mortality in cases of severe PCP (possibly by reducing inflammation due to dying organisms). Indications for corticosteroid use include partial pressure of oxygen (PaO2) <70 mm Hg or an alveolar-arterial (A-a) gradient >35 mm Hg on room air. This patient has a PaO2 of 54 mm Hg on room air, indicating the need for corticosteroid use.
🌆 Community Acquired Pneumonia (CAP)
🏇🏽Streptococcus pneumoniae causes the majority of cases, likely due to increased rates of colonization and impaired immunity against encapsulated bacteria.
Dx: Sputum gram stain and Culture. A Gram stain that shows gram-positive lancet-shaped diplococci intracellularly is good evidence for pneumococcal infection.“Rusty sputum” is classic for pneumococcal pneumonia but may not always be present.
Severe CAP, defined as CAP in a patient who requires admission to an intensive care unit or transfer to an intensive care unit within 24 hours of admission. Blood cultures, Legionella and Streptococcus pneumoniae urine antigen assays, and endotracheal aspirate for Gram stain and culture are recommended for hospitalized patients with severe CAP.
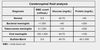
IDSA/ATS Minor Criteria for Severe Community-Acquired Pneumonia
Clinical Criteria
- Confusion (new-onset disorientation to person, place, or time)
- Hypothermia (core temperature <36.0°C [96.8°F])
- Respiration rate ≥30 breaths/mina
- Hypotension necessitating aggressive fluid resuscitation
- Multilobar pulmonary infiltrates
Px: When a portion of the lung is consolidated (eg, lobar pneumonia), the density of tissue/fluid increases and dullness to percussion is detected. In addition, sound conducts more rapidly through the consolidated lung, resulting in increased intensity of breath sounds and a more prominent expiratory component. More rapid sound conduction also results in increased tactile fremitus as well as egophony (sounds like the letter “A” when the patient says the letter “E”) in areas of lung consolidation. Crackles are also often heard.
Laboratory Criteria
- Arterial PO 2/FIO 2 ratio ≤250a
- Leukopenia (<4000 cells/µL )
- Thrombocytopenia (<100,000 platelets /µL)
- Blood urea nitrogen >20 mg/dL
CURB-65 Identifies ❗high-risk patients and to predict a complicated course. Patients who meet at least two criteria are usually admitted to the hospital (mortality rate 8.3%), and those with at least three criteria are considered for intensive care unit (ICU) admission (mortality rate 20%).
Confusion, blood Urea nitrogen >20 mg/dL, Respiration rate ≥30 breaths/min, systolic Blood pressure <90 mm Hg OR diastolic blood pressure <60 mm Hg, and age ≥65 years)
Tx: Pneumococcal 💉vaccination is recommended for all patients with HIV to reduce the risk of invasive S pneumoniae disease. Empirical antibiotic therapy becomes more difficult in community-acquired pneumonia as more pathogens a re recognized and as the pneumococcus develops resistance to penicillin, macrolides, and even quinolones.
(Outpatient): 🐦Macrolide (azithromycin, clarithromycin, or erythromycin) or doxycycline
Risk factor(s) for drug-resistant S. pneumoniae or underlying comorbidities
Respiratory fluoroquinolone (moxifloxacin, gemifloxacin, or levofloxacin) or β-lactam plus a macrolide or doxycycline
Tx: (Inpatient):
Medical ward
β-lactam plus a macrolide or doxycycline; or respiratory fluoroquinolone (eg, moxifloxacin, gemifloxacin or levofloxacin)
Intensive care unit
β-lactam plus either azithromycin or a fluoroquinolone; if penicillin allergic, a respiratory fluoroquinolone plus aztreonam
Modifying Factors That Increase the Risk of Infection With Specific Pathogens
Age >65 y, β-lactam therapy (in previous 3 mo), alcoholism, immunosuppression (illness, glucocorticoids), multiple medical comorbidities, exposure to a child in a day care center
Penicillin-resistant and drug-resistant pneumococci
Residence in an extended care facility, underlying cardiopulmonary disease, multiple medical comorbidities, recent antibiotic therapy
Enteric gram-negative bacteria
Pseudomonas aeruginosa 🛀🏿
Structural lung disease (bronchiectasis), glucocorticoids therapy, broad-spectrum antibiotic therapy for >7 d; malnutrition
Dx: 🧞♀️Pseudomonas aeruginosa or 🏮gram-negative rods on sputum Gram stain
Tx: Antipseudomonal β-lactam with pneumococcal coverage (eg, cefepime, imipenem, meropenem, or piperacillin-tazobactam) ➕ ciprofloxacin or levofloxacin (750 mg) OR antipseudomonal β-lactam with pneumococcal coverage plus an aminoglycoside plus azithromycin; or antipseudomonale β-lactam with pneumococcal coverage plus an aminoglycoside plus a respiratory fluoroquinolone
Endobronchial obstruction (tumor)
Anaerobes, Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus
💉Intravenous drug use
Anaerobes, S. aureus, Mycobacterium tuberculosis, S. pneumoniae
Influenza epidemic in the community
Influenza virus, S. pneumoniae, S. aureus, H. influenzae
COPD, 🚬 smoking history
S. pneumoniae, H. influenzae, Moraxella catarrhalis, P. aeruginosa, Legionella species, Chlamydophila
Poor 🦷dental hygiene, aspiration, lung abscess
Oral anaerobes
Animal exposure
Coxiella burnetii (farm animals); Chlamydophila psittaci, Cryptococcus (birds); Histoplasma (birds, bats)
PR/MDR 💪🏿Pneumococcal Pneumonia
Hx: Age >65 y, β-lactam therapy (in previous 3 mo), alcoholism, immunosuppression (illness, glucocorticoids), multiple medical comorbidities, exposure to a child in a day care center.
Dx: CA-MRSA or compatible sputum Gram stain
Tx: Add 🚐vancomycin OR 🚧 linezolid to β-lactamb ➕ either 🐦azithromycin or a fluoroquinolone.
Patients with bacteremic pneumococcal pneumonia should be discharged on oral amoxicillin to complete 7 days of therapy.
Sinusitis
Rhitnitis
Hx: Facial pain, headache, pressure that incresaes when bending forward, purulent nasal discharge, pus in the nasal cavity, unilateral sinus pain or tenderness, maxillary toothache.
Allergic rhinitis is present in at least 60% of people with recurrent sinusitis.
Dx: sinus CT is rarely necessary (12 weeks)
Tx: Largely symptomatc;
First-generation antihistamine (diphenhydramine)[Benadryl]
Intranasal antihistamine (azelastine, olopatidine)
Intranasal glucocorticoids (Fluticasone [Flonase],
Topical decongestants (Afrin; oxymetazolam) have all been shown to be helpful. Topical decongestants should be limited to a few days of use to avoid rebound rhinitis (rhinitis medicamentosa).
Also try: sinus rinses, inhalation oh humidified air, and adequate hydration.
Criteria for Abx:
- symptoms for 10-14 days
- colored discharge
- sinus pain
Purulent rhinorrhea, purulent secretions in the nasal cavity, tooth pain, and a biphasic history (worsening of symptoms after an initial period of improvement) have been found to be associated with bacterial sinusitis.
Acute bacterial rhinosinusitis
Clinical features
- Cough, nasal discharge
- Fever
- Face pain/headache
Diagnostic criteria (1 of 3)
- Persistent symptoms ≥10 days without improvement
- Severe onset (fever ≥39 C [102.2 F] + drainage) ≥3 days
- Worsening symptoms following initial improvement
Treatment
- Amoxicillin ± clavulanate
Viral URI symptoms typically self-resolve in 7-10 days. In contrast, ABRS is diagnosed by any 1 of the following 3 criteria:
- Symptoms (eg, cough, congestion) persist for ≥10 days without improvement.
OR
- Symptoms severe in onset (fever ≥39 C [102.2 F] + drainage) for ≥3 days.
OR
- Symptoms worsen following initial improvement (ie, biphasic illness). Fever may be absent.
Most cases are due to nontypeable Haemophilus influenzae or Streptococcus pneumoniae. Worsening symptoms (eg, progressive cough ± fever), as seen in this patient, are treated with oral antibiotics (eg, amoxicillin ± clavulanate) at the time of diagnosis. In contrast, in patients with persistent but not worsening symptoms and a milder course, oral antibiotics or a 3-day period of observation for clinical improvement are both acceptable treatment options.
Cx:
Untreated ABRS can lead to life-threatening complications such as periorbital/orbital cellulitis due to orbital extension as well as meningitis or brain abscess due to intracranial extension.
Intracranial complications should be suspected in patients with persistent headache and early-morning vomiting, which occurs due to increased intracranial pressure in the recumbent position. Other findings may include altered mental status (eg, drowsiness), neck pain (suggestive of meningeal irritation), and focal neurologic deficits.
The next step in management is urgent imaging of the brain, orbits, and sinuses. Although MRI is more sensitive, CT scan is faster and can detect early cerebritis; a ring-enhancing lesion confirms the diagnosis. Treatment is intravenous antibiotics and surgical drainage.
Influenza
Influenza virus is largely a winter infection that attacks the epithelium of the upper and lower respiratory tract. Approximately 1-5 days after exposure, patients abruptly develop systemic (fever, malaise, myalgias, headache) and upper/lower respiratory (rhinorrhea, sore throat, nonproductive cough) symptoms. Physical and laboratory examinations are often normal but may show pharyngeal erythema (without exudates) and mild alterations in leukocyte count (low early, high later). Most patients recover spontaneously and completely within 1 week of symptom onset. However, patients with advanced age (>65) and chronic medical illness (eg, coronary artery disease, diabetes mellitus) are far more likely to develop complications.
Sudden onset of high fever (body temperature >39°C [102°F]), severe myalgia, and headache.
Coryza, body temperature up to 41.0°C (105.8°F), myalgia, headache, and sore throat.
Severity of symptoms associated with high fever and myalgia suggest influenza.
Outbreak: In institutional settings such as nursing homes, outbreaks are likely to be particularly severe. Thus, prophylaxis is extremely important in this setting. All residents should receive the influenza vaccine unless they have known egg allergy (patients can choose to decline the vaccine). Since protective antibodies to the vaccine will not develop for 2 weeks, oseltamivir can be used for protection against influenza A during the interim 2-week period. Because of increasing resistance, amantadine is no longer recommended for prophylaxis. The best way to prevent influenza-associated pneumonia is to prevent the outbreak in the first place.
Cx: Pneumonia is the most common complication of influenza and is the result of either secondary bacterial infection (eg, Streptococcus pneumoniae) or direct viral attack (influenza pneumonia). Patients with primary influenza pneumonia typically have an acute worsening of symptoms (dyspnea, cough), leukocytosis (although <15,000/mm3), hypoxia, and bilateral, diffuse interstitial infiltrates on chest x-ray.
Tx: Hospitalization with supplemental oxygen support and antiviral (eg, oseltamivir) treatment is usually required. Influenza may also cause complications in the muscle (myositis, rhabdomyolysis), heart (myocarditis, pericarditis), and central nervous system (encephalitis, transverse myelitis).
Adults at high risk for influenza complications
- Age >65
- Women who are pregnant & up to 2 weeks postpartum
- Underlying chronic medical illness (eg, chronic pulmonary, cardiovascular, renal, hepatic)
- Immunosuppression
- Morbid obesity
- Native Americans
- Nursing home or chronic care facility residents
Actinomycosis
Characterized by cough, hemoptysis, and (eventually) draining sinuses. Has an indolent course; patients may have respiratory symptoms for up to 5 mo before diagnosis. Sulphur granules are seen in stained specimens from draining sinuses.
Blastomycosis
Blastomycosis is a fungal infection that occurs most often in the vicinity of the Great Lakes, 🗺 Mississippi river and Ohio River basins (Wisconsin has the highest infection rate). The pulmonary symptoms and chest x-ray findings of
Blastomycosis presents with signs and symptoms of chronic respiratory infection.
Systemic Blastomycosis may cause characteristic raised, ulcerated skin lesions and lytic bone lesions. The skin lesions in exposed areas become crusted, ulcerated, or verrucous.
Aspergillus
A ubiquitous fungus that most people encounter daily. Conidia are inhaled into the lung and convert to potentially pathogenic hyphae. Patients with immunocompetency rapidly clear the organism and rarely develop infection; however, a subset of immunocompetent patients with a history of pulmonary disease (eg, cavitary tuberculosis) may develop chronic pulmonary aspergillosis (CPA) at sites of lung damage. Diagnosis is made by the presence of all 3 of the following:
>3 months of symptoms - fever, weight loss, fatigue, cough, hemoptysis, and/or dyspnea
Cavitary lesion(s) containing debris, fluid, or an aspergilloma (fungus ball)
Positive Aspergillus IgG serology
Tx: Therapy depends on symptoms and severity of disease; antifungal medication (eg, itraconazole, voriconazole), surgery (to prevent hemoptysis), and bronchial artery embolization (for hemoptysis with extensive disease) may be used together or separately.
Histoplasmosis
Histoplasmosis is an endemic mycosis of the central and midwestern United States that rarely causes illness in immunocompetent individuals but may occasionally cause subacute pulmonary symptoms (<5%).
Histoplasma capsulatum (present as mold in soil and in bird and bat droppings) is endemic to the Mississippi and Ohio River basins. In an appropriate epidemiologic setting, pulmonary histoplasmosis should be considered when pulmonary symptoms are accompanied by mediastinal or hilar lymph nodes (or masses) or by arthralgias and erythema nodosum.
Cx: ❗ Disseminated histoplasmosis in immunocompromised patients can present with lymphadenopathy, pancytopenia, and hepatosplenomegaly as the organism targets histiocytes and the reticuloendothelial system.
Caseating granulomas are most common, but non-caseating granulomas may be the only finding. Careful fungal tissue stains and culture, along with Histoplasmaurinary antigen testing, are used for diagnosis.
Small dose inoculation is rarely symptomatic (<5% become ill); patients who inhale larger doses (eg, exposure in enclosed areas such as a cave) are at higher risk for symptomatic infection. Symptoms usually present 2-4 weeks after exposure with subacute fever, chills, malaise, headache, myalgias, and dry cough.
Chest x-ray typically reveals mediastinal or hilar lymphadenopathy (LAD) with focal, reticulonodular, or miliary infiltrates (depending on the degree of exposure).
Diagnosis is usually made with Histoplasma antigen testing of the urine or blood, plus serology. Some patients may require tissue diagnosis, which often reveals granulomas with narrow-based budding yeasts. Most cases resolve completely (over weeks) without intervention. For patients with moderate or severe disease, oral itraconazole or intravenous liposomal amphotericin B can be used.
Dx: Chest radiography may show a miliary (eg, histoplasmosis) or cavitary lesion.
Coccidioides
Coccidioides is an endemic mold of the desert southwest whose spores are easily aerosolized in the dry months after a rainy season. Inhalation of a single arthroconidium is sufficient to cause infection (usually 7-14 days after inoculation). Symptoms may be subclinical, but many patients (>50%) develop community-acquired pneumonia (CAP) (fever, chest pain, productive cough, lobar infiltrate) often accompanied by arthralgias, erythema nodosum, or erythema multiforme. This clinical syndrome is also called Valley Fever, and symptoms frequently last weeks or months.
Diagnosis should be suspected in any patient living in or traveling to an endemic region (particularly Arizona or California) who has a lower respiratory illness lasting >1 week. Confirmation primarily relies on serologic testing, but cultures are often sent.
Tx: Most patients who are otherwise healthy and have mild or moderate disease do not need antifungal treatment and can have regular follow-up to ensure resolution. However, patients with severe disease or certain risk factors (eg, HIV, immunosuppressive medications, diabetes mellitus) are much more likely to develop dissemination (bones, central nervous system, skin); these patients require antifungal treatment (eg, ketoconazole, fluconazole).
👩🏿🚒Adrenal crisis
Allergic rhinitis
Seasonal nasal symptoms, including clear rhinorrhea and watery, itchy eyes. Patients may have a history of asthma.
Behçet disease
Behçet disease is an uncommon systemic disease with genital ulcers as one component; the ulcers are often painful. Other features include recurrent oral aphthous ulcers, uveitis, pathergy, arthritis, gastrointestinal manifestations, and central nervous system disease. In Behçet disease, serologic tests for syphilis will be negative.
Campylobacter spp.
Poultry, raw milk, travel history
Reactive arthritis can occur after Shigella, Salmonella, and Campylobacter infections.
Guillain-Barré syndrome is associated with Campylobacter and Yersinia infections.
💊 Cephalosporins
First generation Active against most gram-positive cocci (including penicillinase-producing staphylococci).
Cefazolin (Ancef, Kefzol) IV
Cephalexin (Keflex, Biocef, Keftab) PO
Second generation greater activity against certain gram-negative bacilli; specifically, one subgroup of second-generation cephalosporins has enhanced activity against H. influenzae
Cefuroxime (Kefurox, Zinacef)
Cefotetan (Cefotan)
Cefoxitin (Mefoxin)
Third generation The third-generation cephalosporins are less active against most gram-positive organisms than the first-generation cephalosporins. Highly active against Enterobacteriaceae (E. coli, Proteus mirabilis, indole-positive Proteus, Klebsiella, Enterobacter, Serratia, Citrobacter), Neisseria, and H. influenzae. They are the therapy of choice for gram-negative meningitis due to susceptible Enterobacteriaceae.
Ceftriaxone (Rocephin) has the longest serum half-life of this group (6.4 hours) and can be administered once or twice a day.
Cefotaxime (Claforan)
Ceftazidime (Fortaz) 🧞♀️
Fourth generation
Cefepime (Maxipime) 🧞♀️
Advanced generation and combination agents
Ceftaroline (Teflaro) improved gram-positive activity. activity against MRSA,
Fluoroquinolones
Fluoroquinolones upregulate cell matrix metalloproteases, leading to increased collagen degradation; this mechanism is likely responsible for several associated adverse effects, including Achilles tendon rupture, retinal detachment, and aortic aneurysm rupture.
The increased risk of aortic aneurysm rupture with fluoroquinolones is small overall, but it warrants serious consideration due to the high morbidity and mortality of rupture. Hence, when possible, these drugs should be avoided in patients with known aortic aneurysm or substantial risk factors for aortic aneurysm (eg, Marfan syndrome, Ehlers-Danlos syndrome, advanced atherosclerotic disease, uncontrolled hypertension).
Other adverse effects of fluoroquinolones that are likely unrelated to collagen degradation include encephalopathy, peripheral neuropathy, and QT-interval prolongation.
🦠 Chlamydia / Gonorrhea
Acute cervicitis is most commonly caused by Chlamydia trachomatis and Neisseria gonorrhoeae. Infection by these pathogens is most prevalent in women age <25. Acute cervicitis is diagnosed clinically by a pelvic examination that shows a mucopurulent discharge and a friable cervix (eg, bleeds easily on contact). Treatment is empiric with azithromycin and ceftriaxone, but nucleic acid amplification testing should also be performed for infection confirmation.
Risk factors
- Age <25
- High-risk sexual behavior
Manifestations
- Asymptomatic (most common)
- Cervicitis
- Urethritis
- Perihepatitis (Fitz-Hugh-Curtis syndrome)
Mucopurulent cervicitis with exacerbation during and after menstruation is classic gonorrhea.
Diagnosis
- Nucleic acid amplification testing
Treatment
- Empiric: 🐦Azithromycin + 🔨ceftriaxone (Rocephin)
- Confirmed Gonorrhea: 🐦Azithromycin + 🔨ceftriaxone OR 🌼 floroquinolone
- Confirmed Chlamydia: 🐦Azithromycin OR 🎡Doxycycline (Ceftriaxone is NOT for Chlamydia)
- Azithromycin 1 g orally, given in a single dose or doxycycline 100 mg orally twice daily for 7 d
👓 Spectinomycin is the treatment of choice for pregnant women who have asymptomatic N. gonorrhoeae infections and who are allergic to penicillin. 🐓 Erythromycin is another drug that is effective.
Complications
- Pelvic inflammatory disease
- Ectopic pregnancy
- Infertility
- Pharyngitis
Tx:
Gonorrhea would be described as a ⚪ clearer cervical discharge (“not so mucopurulent”) and excluded by a gram stain with culture.
Chlamydia generates a mucopurulent 💛 yellow cervical discharge
Disseminated gonococcal infection
Disseminated gonococcal infection
- Purulent monoarthritis OR Triad of tenosynovitis, dermatitis, migratory polyarthralgia
Diagnosis
- Detection of Neisseria gonorrhoeaein urine, cervical, or urethral sample
- Culture of blood, synovial fluid (less sensitive)
Treatment
- 3rd-generation cephalosporin IV AND oral azithromyci
Migratory joint symptoms and often have involvement of several joints with tenosynovitis.
Skin lesions are found in more than 75% of patients with DGI but may be few in number; consequently. Lesions are most likely to be found on the extremities. The classic lesion is characterized by a small number of necrotic vesicopustules on an erythematous base.
Dx: Nucleic acid amplification urine test (NAAT) for Neisseria gonorrhoeae is a noninvasive, sensitive test for diagnosing gonorrhea in men. This test provides rapid results (within hours) and can help to guide therapy pending return of blood and synovial fluid culture results.
Mucosal cultures, including of the throat, anus, urethra, or cervix (in women), may also be helpful in establishing the diagnosis.
Tx: Infection of cervix, urethra, or rectum:
Ceftriaxone 125 mg IM, given in a single dose, PLUS either azithromycin 1 g orally in a single dose or doxycycline 100 mg orally twice daily for 7 days
Trachoma
Trachoma is due to Chlamydia trachomatis serotypes A, B, and C and is the leading cause of blindness worldwide. C trachomatis spreads effectively in crowded or unsanitary conditions. The active phase is most common in children and is characterized by follicular conjunctivitis and pannus (neovascularization) formation in the cornea. There is often a concomitant nasopharyngeal infection (eg, rhinorrhea, pharyngitis). Repeated or chronic infection leads to scarring of the eyelids and inversion of the eyelashes (trichiasis). Over time, the lashes rub on the eye and cause ulcerations and blindness (cicatricial trachoma).
The diagnosis can be made clinically by examination of the tarsal conjunctivae. C trachomatis may be visible by Giemsa stain examination of conjunctival scrapings. Oral azithromycin is effective against C trachomatis; in general, the entire region (eg, village, refugee camp) should be treated simultaneously. For individuals with trichiasis, eyelid surgery is needed to preserve vision.
Reactive arthritis
Reactive arthritis is a type of seronegative spondyloarthropathy. Reactive arthritis occurs in both men and women, and enthesitis and oligoarthritis are common.
Classic reactive arthritis consists of a triad of nongonococcal urethritis, asymmetric oligoarthritis and conjunctivitis. The arthritis often involves the knee and sacroiliac spine.
Hx: The classic triad of arthritis, urethritis, and conjunctivitis occurs in only about one third of patients.
Manifests within 2 months of an episode of bacterial gastroenteritis or n_ongonococcal urethritis_ or cervicitis in a genetically predisposed patient.
Reactive arthritis was previously called Reiter syndrome, which referred to the coincidence of arthritis, conjunctivitis, and urethritis (or cervicitis). However, only about one third of patients have all three symptoms.
Reactive arthritis usually affects the peripheral joints, often in the lower extremities, although inflammatory back pain also may be present.
Patients may also present with heel pain with enthesitis; keratoderma blennorrhagicum on the palms or soles; or circinate balanitis on the penis.
Differs from rheumatoid arthritis in that it is oligoarticular and asymmetric?
Presents as symmetric? inflammatory oligoarthritis, most often involving weight-bearing joints; may include tendon insertion inflammation (enthesitis).
Extra-articular manifestations include conjunctivitis, urethritis, stomatitis, and psoriaform skin changes (hyperkeratotic lesions on the palms and soles). Infection with Salmonella, Shigella, Yersinia, Campylobacter, or Chlamydia species within 3 wk prior to onset of initial attack.
Synovial fluid analysis is usually sterile. 🧯 Nonsteroidal anti-inflammatory agents (NSAIDs) are the first line therapy during the acute phase of this condition.