Vascular Pathology I Flashcards
(43 cards)
Ischaemia
deficiency of O2’d blood in a tissue causing impaired aerobic respiration and cell death
Hypoxia
deficiency of oxygen in tissues
Hypoxemia
deficiency of oxygen in blood
Infarct
area of necrosis caused by acute ischemia
Thrombus
clotted blood within the cardiovascular system
Embolus
intravascular solid, liquid, or gaseous mass carried in blood stream to some site remote from its origin (e.g. detached thrombus, CO2 poisoning in diving)
Atherosclerosis
- underlying disease of most CVD
- accumulation of lipid and fbirous CT = plaque
- intima of MEDIUM and LARGE ARTERIES
- caused by endothelial dysfunction and chronic inflammation
Risk factors for artherosclerosis include
- High blood lipids
- high BP
- smoking
- age
- sex
- genetics
- diabetes (diabetic dyslipidaemia: altered balance of HDL & LDL; smaller denser LDL)
- lipoproteins (genetics, diet) e.g. elevated LDL, VLDL
- obesity, metabolic syndrome
- proteinuria
What does dysfunctional endothelium lead to?
Increased permeability to LDL in blood
decreased production of NO (vasodilation) and prostacyclin (PGI2, inhibiton of platelet aggregation)
What are the 5 main classes of lipoproteins?
- chylomicrons
- very low density L
- LDL
- intermediate DL
- high DL
What happens when LDL enters the intima?
oxidized by ROS
trapped
inflammatory response
IL-8 –> macrophages
phagocytosed –> foam cells



What is the consequence of media smooth muscle cells migrating to the intima?
(due to PDGF, TGF-b, cytokines from macrophages, etc.)
generates ECM inside the intima

Where does lipid accumulate from in the plaque?
breakdown of foam cells
cholesterol from cell membranes (form cyrstals)

What contributes to increased disease risk (e.g. atherosclerosis, type II diabetes, hypertension, fatty liver disease) in metabolic syndrome?
cytokines and growth factors released from adipose tissue interfere with insulin signalling and BP regulation




What cell type is this?

Foam cells: macrophages with foamy cytoplasm from phagocytosed LDL
What are 3 major complications of atherosclerosis?
Ischaemia
Infafction
Aneurysm
What is the mechanism by which atherosclerotic plaque leads to aneurysm?
- placque buildup in intima puts pressure on media, imparing O2 saturation (usually by lumen)
- media atrophies and weakens and dilates
- leads to aneurysm
- possible thrombus, thrombo-embolis formation, rupture
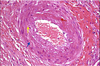
What atheroscleortic complication is this?

Fixed vessel narrowing (coronary artery)
Red circle denotes normal lumen size
H&E: fibrous placque (not as much lipid as L)
What are important sites of atherosclerosis?
- abdo aorta (AAAs most common)
- corontary arteries (lead to CVAs, infarcts)
- femoral arteries, popliteal
- kidnes (renal arteries)
- mesenteric arteries (small bowel)
What is the character of a true/fusiform anuerysm?
entire circumference of vessel wall is dilated

What type of aneurysm is this?

True/fusiform
complete circumferential dilation