W6 - Circulation (2.6) Flashcards
What are the functions of the circulatory system?
transport of
- nutrition, O2, CO2, metabolites
- thermoregulation (= transport of heat)
- hormones (= endocrinological function)
- cells of immune system (= immunological function)
What is the two-pump system?
Explain.
simplified model for cardiovascular system
- 2 pumps in series: right, left ventricle
- 2 vascular beds in series: systemic, pulmonary vasculature
→ flow pumped in both systems virtually equal to each other

Elaborate on the following parameters of the aorta:
- diameter, thickness of wall
- amount of elastic tissue
- amount of smooth mm.
- number
- cross sectional area [cm2]
- percentage of blood volume

Elaborate on the following parameters of arteries:
- diameter, thickness of wall
- amount of elastic tissue
- amount of smooth mm.
- number
- cross sectional area [cm2]
- percentage of blood volume
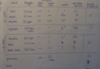
Elaborate on the following parameters of arterioles:
- diameter, thickness of wall
- amount of elastic tissue
- amount of smooth mm.
- number
- cross sectional area [cm2]
- percentage of blood volume
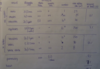
Elaborate on the following parameters of capillaries:
- diameter, thickness of wall
- amount of elastic tissue
- amount of smooth mm.
- number
- cross sectional area [cm2]
- percentage of blood volume

Elaborate on the following parameters of venules:
- diameter, thickness of wall
- amount of elastic tissue
- amount of smooth mm.
- number
- cross sectional area [cm2]
- percentage of blood volume
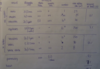
Elaborate on the following parameters of veins:
- diameter, thickness of wall
- amount of elastic tissue
- amount of smooth mm.
- number
- cross sectional area [cm2]
- percentage of blood volume
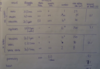
Elaborate on the following parameters of the vv. cavae:
- diameter, thickness of wall
- amount of elastic tissue
- amount of smooth mm.
- number
- cross sectional area [cm2]
- percentage of blood volume
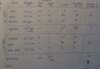
Elaborate on the following parameters of the vessels of the pulmonary circulation:
- amount of elastic tissue
- amount of smooth mm.
- percentage of blood volume
What percentage of blood volume can be found in the heart?
7%
→ approx. 350 - 450 ml
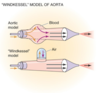
Although hemodynamics are a powerful tool to describe physics of blood/fluid flow through the circulatory system, they are not 100% exact.
Why is that?
bc in vessels
- flow is pulsatile: pressure P, flow Q are not constant
- wall is not rigid due to el. tissue: radius r, cross sectional area A can be changed
- blood is a non-newtonian fluid: velocity v is not always constant
Explain the relationship btw velocity and the cross-sectional area.
equation of continuity
conservation of mass causes fluid flow to be constant in every 2 sections of a tube
→ velocity inversely proportional to cross-sectional area
Q = A * v
A * v = constant
BUT: same applies if A2 is spread among many vessels

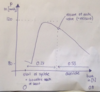
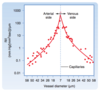
Relate the velocity-cross-sectional area relationship in a graph.
- velocity decreases in arterial system
- minimal value in capillaries
- velocity increases in venous system

What does the lowest point of the velocity graph indicate?
Value?

lowest v (= 0.3 mm/s) in capillaries → **longest time (1 - 3s) for diffusion btw circulatory system and peripheral tissues**
What are the types of pressure in a tube?
- static pressure Pstat: pressure if fluid is not moving or if object is moving w/ the fluid dynamic pressure Pdyn: pressure of a fluid that results from its motion
→ Pstat + Pdyn = Ptotal
lecture guy referred to static pressure as side pressure
How can dynamic pressure be calculated?
dynamic pressure is directly proportional to density and velocity
Pdyn = 1/2 ⍴ v2
- ⍴ = density
- v = velocity
BUT: usually negligible in most arterial locations
Describe the effect of velocity on static pressure in a tube.
Which law describes this relationship?
- *Bernoulli’s law** states that if the v is increased a decreased Pstat can be measured
- *↑v → ↓Pstat**
because:
- ↑v → ↑Pdyn
- Pstat + Pdyn = Ptotal
- conservation of E
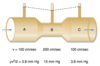
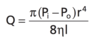
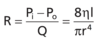
Which relationship is described by Hagen-Poiseuille’s law?
Formula.
describes flow of fluid in terms of
- ΔP (Pi - Po) = pressure gradient btw inlet and outlet
- r = radius of the tube
- ƞ = viscosity of the fluid
- l = length of the tube
NOTE: radius is the critical factor
(raised to the 4th power)
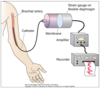
Give the formula for hydraulic resistance in fluid mechanics.
ability of vessels to fluid flow
R = ΔP/Q
- ΔP = pressure gradient btw inlet and outlet of tube
- Q = flow
⇒ resistance is inversely proportional to fluid flow
How can the resistance of vessels be calculated using Hagen-Poiseuille’s law?
Formula + unit.
Hagen’s Poiseuille’s law can be plugged in to formula for hydraulic resistance to substitute fluid flow, pressure gradient can be cancelled out
in [R unit] (instead of mmHg*sec/ml)
- ƞ = viscosity of fluid
- l = length of tube
- r = radius of tube
NOTE: radius is the critical factor
(raised to the 4th power)
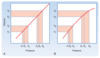
What is the consequence of Hagen-Poiseuille’s law w/r/t the resistance in various blood vessels?
depends mainly on vessel diameter
- highest resistance in capillaries
- diminishes as vessels incr. in diameter on art./ven. sides of capillaries
Name 2 mechanisms that can change the diameter of a vessel.
- contraction of circular smooth mm. in the vessel wall
- transmural pressure = pressure difference btw int./ext. pressure, hence ↑Pint w/o incr. Pext → dilation of vessel
How can resistances in series and parallel be calculated?
in series: RT = R1 + R2 + R3 + …
in parallel: 1/RT = 1/R1 + 1/R2 + 1/R3 + …
⇒ total resistance = less than individual resistances bc additional pathways for fluid flow are provided
NOTE: RT = total peripheral resistance