Week 1 Flashcards
(106 cards)
What are the components of…
- the upper urinary tract
- the lower urinary tract?
Upper - left and right kidneys, left and right ureters
Lower - bladder and urethra
What part of the urinary tract is included in the following areas?
- abdomen
- pelvis
- perineum
Abdomen - kidneys, proximal ureters
Pelvis - distal ureters, bladder, proximal urethra
Perineum - distal urethra
The kidneys are intra/retroperitoneal
The great vessels (IVC and aorta) are intra/retroperitoneal
Kidneys are retroperitoneal
Great vessels are also retroperitoneal
What are the three structures of the renal hilum? Which of these structures always sits most anteriorly?
Renal artery
Renal vein - always sits anteriorly
Ureter

From superficial to deep, what layers surround the kidney to the peritoneum? (5)
Visceral peritoneum
Paranephric fat
Renal (deep) fascia
Perinephric fat
Renal capsule

What muscle sits medially to the kidney?
What muscle sits posteriorly to the kidney?
The Psoas major sits medially
The Quadratus lumborum sits posteriorly
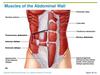
What are the three layers of abdominal wall muscle?
External oblique
Internal oblique
Transversus abdominis
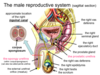
Where do the following drain to…
- Renal artery
- Renal vein
Artery - abdominal aorta
Vein - IVC
At what vertebral level are the kindeys (right and left are at different levels!)
Right - L1-L3
Left - T12-L2

When attempting to ballot the kidneys, what should you ask the patient to do? Why?
Ask the patient to breathe in.
As the liver and spleen lie in direct contact with the diaphragm, when the patient breathes in this expands the lungs and pushes these organs down. The liver and spleen are also in contact with the kindeys, so on inspiration they too are pushed down and may be “trapped” on balloting
What is the name of the recess where fluid would collect if a patient was supine?
The hepatorenal recess between the kidney and the liver
At what level does the abdominal aorta bifurcate?
What happens to the relationship between the arteries and veins at this point?
The abdominal aorta bifurcates at the level of the umbilicus (L3-L4)
While the renal arteries are posterior to the renal veins, the common iliac arteries are anterior to the common iliac veins

Where does the lymph from the a) kidneys and b) ureters drain to?
a) lymph from the kidneys drains to the lumbar nodes (located around the great vessels)
b) lymph from the ureters drains to both the lumbar and the iliac nodes
What’s the difference between a supra-renal and infra-renal AAA?
Supra-renal AAAs include the renal arteries, and renal artery stenosis is a result of the AAA (aneurysm narrows and occludes artery)
Infra-renal AAAs are below the renal arteries, and renal artery stenosis may be combined with the AAA (both caused by atherosclerosis)

What anatomical variations may be seen in kidney development?
Bifid renal pelvis
Bifid ureter and unilateral duplicated ureter
Retrocaval ureter
Horseshoe kidney
Ectopic pelvic kidney
What are the two main parts of the kidney contained within the renal capsule?
Where are the nephrons contained?
- The cortex
- The medulla
Nephrons are contained in renal pyramids, which are contained within the medulla

Proximally to distally, what are the various structures of a nephron?
Glomerulus
Proximal convoluted tubule
Loop of Henle
Distal convoluted tubule
Collecting duct
Minor calyx

Describe the drainage of urine from the kidney to the ureter.
At what point is the first constriction in this pathway?
Nephron collecting ducts > minor calyx > major calyx > renal pelvis > ureter
The diameter of these structures continues to increase until the pelviureteric junction (where the renal pelvis becomes the ureter)
What are the three sites of ureteric constriction?
Why are these clinically important?
- Pelviureteric junction
- Ureter crossing the anterior aspect of the common iliac artery
- Ureteric orifice into the bladder (corner of the trigone)
Clinical importance - this is where kidney stones will most likely cause issue
Why is there a colicky pain associated with kidney stones?
The ureters have a peristaltic motion. Upon obstruction, there is increased peristalsis proximally to the site of the blockage
What is hydronephrosis? What causes it?
“Water inside the kidney”, caused by back pressure of urine into calyces, which compresses the nephrons and results in renal failure.
Acutely painful
What are the different areas of the pelvic cavity? What structures form the boundaries between these areas?
False pelvis - from the iliac crests to the pelvic inlet, contains abdominal organs
True pelvis - pelvic inlet to pelvic floor, contains pelvic viscera
Perineum
False pelvis and True pelvis are separated by the pelvic rim (inlet), True pelvis and Perineum are separated by the pelvic floor, specifically the levator ani

What structures pass through the pelvic floor?
Distal parts of the alimentary (rectum), renal (bladder) and reproductive tracts
Describe the path of the ureters from the abdominal cavity to the bladder. At what point to they turn medially?
Leave the kidney, travel inferiorly and pass anteriorly to the common iliac vessels to enter the pelvis
Run anteriorly, along the lateral walls of the pelvis
At the level of the ischial spine the ureters turn medially to enter the posterior aspect of the bladder