Week 3/4 - E - Pneumonia (Symptoms, Ix, CURB65, C.A.P, H.A.P, Atypical) and TB (pathogenesis/latent/active/diagnosis/treatment) Flashcards
(46 cards)
Pneumonia is an acute lower respiratory tract infection causing inflammation of the lung tissue, primarily the alveoli What are the symptoms of pneumonia and what patients can present in atypical ways?

Symptoms * Fevers * Sweats * Rigors * Cough * Dyspnoea * Confusion * Haemoptosis * Pleuritic pain * Confusion - may be the only sign in the elderly
What are the signs of pneumonia?
Cyanosis - could be in resp failure Tachypnoea Chest expansion - reduced Percussion note - dull Auscultation - crackles Also may have hypotension
There are different investigations that can be carried out for pneumonia What investigations would usually be carried out in a patient admitted to hospital?
Assess oxygenation - if O2 sats <92%, then ABG Blood tests - FBC, U&Es CXR looking for new infiltrates in the lung or pleural effusion

Do not routinely offer microbiological tests to patients with low‑severity community‑acquired pneumonia. When are tests offered and what are the microbiological tests?
For patients with moderate‑ or high‑severity community‑acquired pneumonia: take blood and sputum cultures and consider pneumococcal and legionella urinary antigen tests.
When in hospital, usually a CXR is used to assists in the diagnosis of pneumonia in a patient When a clinical diagnosis of community-acquired pneumonia is made in primary care, Use clinical judgement in conjunction with the CRB65 score to inform decisions about whether patients need hospital assessment What score warrants treatment in the community and what score would you advice admittance to hospital?
Patients with a CRB65 score in the community of 0or1 can usually be treated in primary care Patients with a CRB65 score of 2 and above usually require hospital therapy
What is the CRB65 (CURB65 if in hospital) criteria What score is mild/moderate and what score is severe? The score helps to determine the patients mortality risk and the treatment therapy is advised based on this
- CONFUSION, NEW (MSQ ≤8/10)
- UREA >7mmol/l (if available)
- RESPIRATORY RATE ≥ 30/minute
- BP <90mmHg (systolic) or ≤60mmHg (diastolic)
- 65 AGE ≥ 65 years
Mild 0-1
Moderate score = 0-2
Severe score = 3-5

What are the different causative organisms for mild/moderate community acquired pneumonia and what is the treatment (also if pen allergic)?
Mild/moderate community acquired pneumonia * Strep pneumonia and haemophilus influenza B * Treatment - * Amoxicillin PO?IV * If pen allergic - doxycycline or clarithromycin IV if NBM
What are the different causative organisms for severe community acquired pneumonia and what is the treatment (also if pen allergic)?
Severe community acquired pneumonia * Also strep pneumonia and haemophilus influenza B but possible coliforms and atypicals (eg legionella, mycoplasma, chlamydophila, coxiella) * Treatment * IV Co-amoxiclav + PO DOxycycline / IV Clarithromycin if NBM * If pen allergic - IV Levoflaxacin monotherapy
What is hospital acquired pneumonia defined as?
Hospital-acquired pneumonia (HAP) is an acute lower respiratory tract infection that is by definition acquired after at least 48 hours of admission to hospital and is not incubating at the time of admission
What are the causative organisms in hospital acquired pneumonia?
Caused by pneumococcus, haemophilus and coliforms - legionella can also be hospital acuired
What is the treatment of hospital acquired pneumonia, severe and non severe?
Non sevre * Amoxicillin PO * Pen-allergic - Doxycycline Severe * IV amoxicillin + Gentamicin * Pen-allergic - IV CO-trimoxazole + Gentamicin
Aspiration pneumonia Which patients is this more common in? What organisms are important to cover in this type?
Aspiration pneumonia results from inhalation of oropharyngeal contents into the lower airways that leads to lung injury and resultant bacterial infection - eg strokes, muscular palsies, decreased consciouness eg intoxicated or post-ictal Important to cover anaerobes in the treatment
Which bacteria often seen in aspiration lobar pneumonia in alcoholics causes a red-current jelly type sputum? Which bacteria is the commonest cause of community acquired pneumonia and what type of sputum does it cause?
Klebsiella pneumonia - redcurrent jelly sputum Streptococcus pneumonia (pneumococcus)- causes a rsuty coloured sputum
What is the treatment of aspiration pneumonia in non severe and sevre patients?
Non severe - amoxicillin + metronidazole PO Severe - Amox, metron and gent IV If pen allergic -replace amoxicillin with doxycylcine PO or Clarithrmoycin IV
Atypical bacterial pneumonia is caused by atypical organisms that are not detectable on Gram stain and cannot be cultured using standard methods. Name the atypical causes of pneumonia How are they treated?
Legionella pneumonia - levoflaxacin (or macrolide eg clarithromycin) All can be treated with tetracycline eg doxycycline or macrolide eg clarithromycin * Mycoplasma pneumonia * Chlamydophila pneumonia * Chlamydophila psittaci * Coxiella pneumonia
Legionella pneumonia usually colonizes water tanks kept at less than 60 degrees What is the classicial scenario in when a patient gets this disease? What are the symptoms?
Legionella typically occurs in patient returning from holiday with poor air conditioning Symptoms are typically flu like followed by a dry cough GI disturbance and confusion are common
How is legionella pneumonia diagnosed and what is the treatmnet?
Diagnosed with urine antigen test for legionella Treatment - levofloaxacin (fluoroquinolone) or clarithromycin (macrolide)
All can be treated with tetracycline eg doxycycline or macrolide eg clarithromycin * Mycoplasma pneumonia * Chlamydophila pneumonia * Chlamydophila psittaci * Coxiella pneumonia Which atypical bacteria causing pneumonia can result in the autoimmune haemolytic anaemia due to the presence of cold agglutins? Describe this disease and its symptoms
MYCOPLASMA PNEUMONIA Cold agglutinin disease (CAD) is a rare autoimmune disease characterized by the presence of high concentrations of circulating cold sensitive antibodies, usually IgM and autoantibodies that are also active at temperatures below 30 °C (86 °F), directed against red blood cells, causing them to agglutinate and undergo lysis Symptoms of CAD include symptoms of anaemia as well as jaundice and dark urine due to excess bilirubin
As noted, mycoplasma pneumonia can cause an autoimmune haemolytic anaemia due to the presence of cold agglutins WHen does mycoplasma pneumonia typically occur?
Mycoplasma pneumonia typically occurs in epidemics about every 4 years Symptoms include that of anaemia, dark urine, jaundice and pneuomina

How are mycoplasma pneumonia, chlamydophila pneumonia coxiella burnetti diagnosed?
These atypical pneumonias can be diagnosed via serology (bloods taken) howver PCR testing of sputum samples is faster
Which atypical pneumonia is linked to sheep and goats? Which atypical pneumonia is linked to parrots and budgies? What type of sputum does it cause?
Coxiella burnetti- sheeps and goats Chlamydophila psittaci - parrots and budgies - mucoid sputum
What increases the risk of complications in a patient with pneumonia? What are common complications that can arise due to pneumonia?
The risk of complications in a patient with pneumonia increase in the elderly and those with underying health conditions Common complications Type 1 respiratory failure - V/Q mismatch Pleural effusion - that can beocme infected, can cause pus, can cause an intrapulmonary abscess Sepsis
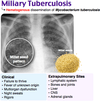
What is tuberculosis and what are the two bacterial pathogens in humans?
Tuberculosis (TB) is a bacterial infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria. Tuberculosis generally affects the lungs, but can also affect other parts of the body. Uusally caused by mycobacteriam tuberculosis but can also be caused by mycobacterium bovis
Mycobacterium tuberculosis usually stains very weakly or not at all on gram staining If it does stain, what does it show?
If the bacteria does stain, it will show rod shaped gram positive bacilli Pink for gram positive