04.06 and 04.07 - Vascular Disease, Aneurysms, Dissections, Vasculitis, etc. Flashcards
(83 cards)
What are the 5 main components of arteries that we should be aware of?
- Tunica intima: inner layer (lining)
- Tunica media: middle layer (smooth muscle)
- Tunica adventitia: outer layer
- Internal elastic lamina: mem separating intima and media
- Vasa vasorum: small blood vessels in tunica media and adventitia of arteries so large that oxygen and nutrients can’t reach these layers by diffusion from lumen
What are 3 important types of arteries?

- Elastic: largest aa (aorta, innominate/braciocephalic, subclavian, common carotid, iliac, pulmonary)
- Muscular: medium size aa (>0.2cm in diameter), incl coronary cerebral, renal, hepatic, femoral, popliteal
- Arterioles: smallest aa (20-100 microns in diameter)
What is an arteriovenous fistula?
Direct connections between aa and vv bypassing intervening capillary bed
What is fibromuscular dysplasia?
- Focal, irregular arterial wall thickening with intimal and medial hyperplasia and fibrosis leading to luminal stenosis (narrowing)
- Presumptively due to developmental disordered growth (NOT pre neoplastic!!)
- Typically in renal, carotid, splanchnic or vertebral aa
- Most commonly diagnosed in young women
What are hyperplastic and hyaline arteriolosclerosis?
- Hyperplastic: concentric wall thickening due to smooth muscle cell hyperplasia and hypertrophy, and thickened reduplicated basement membrane (caused by HTN and causes luminal narrowing; can resemble onion skin)
-
Hyaline: wall thickening due to leakage of plasma protein into wall and increased secretion of matrix by smooth muscle cells (caused by HTN)
1. Differential diagnosis: amyloidosis or fibrinoid change/necrosis
What are fibrinoid change and medial calcific sclerosis?
- Fibrinoid change/necrosis: leakage of plasma protein into wall +/- necrosis (caused by malignant hypertension or vasculitis)
- Medial calcific sclerosis: degenerative calcification of internal elastic lamina, spreading into tunica media, not thought to be clinically significant by itself
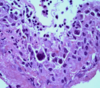
What do you see here? What might have cause this?

- Onion-skin appearance of arteriole with hyperplastic arteriolosclerosis likely due to HTN
- Scleroderma causes similar onion-skin thickening, but of larger, interlobar renal arteries
- Fibromuscular dysplasia causes similar causes similar thickening, but of larger renal arteries outside the renal parenchyma
What do you see here? What are some likely causes?

- Smooth homogenous thickening of an arteriole with hyaline arteriolosclerosis likely due to HTN
- Amyloidosis causes similar appearance, but not limited to arterioles
- Fibrinoid change/necrosis has similar appearance, but often part of vasculitis
What do you see here?

Fibrinoid change
What do you see here?

- Fibrinoid necrosis
- Due to polyarteritis nodosa; not all the vasculitis and surrounding inflammation
What do you see here?

Medial calcific sclerosis (may play a role in devo of temporal giant cell arteritis)
What is this?

- Medial calcific sclerosis
- With intimal thickening, presumably due to separate atherosclerosis, since medial calcific sclerosis occurs in old people, who always also have atherosclerosis
What is an aneurysm?
Discrete, localized dilatation (outpouching) of blood vessel or heart
What is a dissection?
Tear of the tunica intima, letting luminal blood under high pressure into the tunica media, where it tunnels (dissects) a second lumen
What is an ectasia?
Non-discrete, non-localized dilatation, often torturous, of blood vessel or duct
What is Marfan syndrome?
- FBN1 gene for fibrillin-1; auto dom; 1 in 5000
- Abnormal fibrillin & excessive activation of TGF-beta bc normal microfibrils sequester TGF-beta
- Causes cystic medionecrosis of ascending aorta, leading to dilation, predisposing to aortic dissection (cause of death in up to 45% of cases); tall body
- Mainstay of treatment = administration of beta-blockers (which reduce HR, BP and aortic wall stress); angiotensin-2 receptor blockade promising new tx
- Fibrillin: EC glycoproteins responsible for structuring elastin fibers
What is Ehlers-Danlos syndrome?
- Clinically and genetically heterogeneous group of inherited disorders due to defects in synthesis or structure of fibrillar collagen
- Vascular types involve COL3A1 gene for type III collagen
1. Usually auto dom, and have spontaneous rupture of blood vessels and intestines bc rich in type III collagen
What are cystic medial degeneration and vasculitis?

- Cystic medial degeneration: loss of smooth muscle cells and elastic fibers in tunica media of large arteries
- Vasculitis: inflammation of blood vessels
What are the epi, patho, and causes of aortic aneurysms?
-
Epi: common, esp in elderly, white M; run in families
1. Associated w/smoking, HTN, hyperlipidemia -
Patho: interplay b/t atherosclerosis & genetically determined degeneration of tunica media
1. Increased matrix metalloproteinases +/- DEC tissue inhibitors of them
2. Spillover inflammation from atherosclerosis -
Less common causes:
1. Genetic defects in fibrillin or collagen (Marfan)
2. Infection (called mycotic, even when not fungal, which is most of the time)
3. Vasculitis (autoimmune, e.g. giant cell arteritis)
What is this?

- Aortic aneurysm from superior mesenteric artery (bottom) to bifurcation (top)
- Cut edge of aorta: black line = normal circumference
- Variegated brown, mural thrombus
- More common in the abdomen (75%), and thrombus usually forms in it
What is the arrow pointing to?

- Cystic medial degeneration in tunica media (used to be called necrosis) = loss of smooth muscle cells and elastic fibers, leaving cystic areas of myxoid matrix
- Common in aortic aneurysm
What is the difference between left and right?

- Left: elastic stain of aortic tunica media at edge of area of cystic medial degeneration
- Right: elastic stain of aortic tunica media in area with normal elastic fiber density
What are the symptoms, signs, diagnosis, and treatment for aortic aneurysms?
- Symptoms: usually none, but may cause back pain (especially if leaking)
- Signs: usually none
- Diagnosis: imaging
- Treatment: stenting or open repair
What are some complications of aortic aneurysm?

- Rupture: major determinant = diameter
- Mural thrombus formation
- Embolism of atheroma or thrombus
- Obstruction of aortic branches
- Aortoenteric fistula