12. Drug Interactions 2 Flashcards
What do pharmacokinetic drug interactions involve interactions relating to?
Pharmacokinetic Interactions
- Pharmacokinetic drug interactions involve interactions relating to:
- absorption
- distribution
- metabolism
- excretion
What are 2 examples of Pharmacokinetic Interactions that affect Absorption?
Pharmacokinetic Interactions - Absorption
-
Proton pump inhibitors, H2 receptor blocking agents and antacids
- these medications increase gastric pH (reduce acidity) = reduced gastric acid
- may reduce the absorption of some agents e.g. calcium carbonate
-
Calcium supplements and iron preparations reduce the absorption of some agents e.g. alendronate and doxycycline (tetracycline)
- Ca2+/Fe bind to these drugs + the complex then becomes unabsorbable
- Take drugs one hour before, or two hours after calcium supplements or iron preparations
- Eg. Fosamax (for osteoporosis) should not be taken at the same time as Ca2+ supplements

What is the most common type of Pharmacokinetic Interaction?
Pharmacokinetic Interactions – Metabolism = most common pharmacokinetic interaction
What is the most important enzyme system for drug metabolism?
Where is this primarily located?
Cytochrome P450 System
- The most important enzyme system is the Cytochrome P450 System which is located primarily in the liver, and in the gut
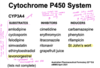
- Is composed of numerous enzymes e.g. CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4
- Many medicines are metabolised by this system, and some medicines are metabolised by more than one P450 enzyme
- Although these enzymes metabolise many drugs (substrates), they may also be inhibited or induced by other drugs
What are some examples of substrates, inhibitors and inducers of the CYP3A4 enzyme of the Cytochrome P450 System?
3 examples of pharmacokinetic drug interactions?
Pharmacokinetic Interactions – Metabolism - Cytochrome P450 System
- Oral Contraceptives + St John’s Wort
- Simvastatin + potent CYP3A4 inhibitors
- eg. erythromycin, itraconazole and ritonavir
- Grapefruit juice + Felodipine
What is the problem with taking St Johns Wort whilst on the oral contraceptive pill?
Interaction Between Oral Contraceptives and St John’s Wort
- The combined oral contraceptive pill contains ethinyloestradiol and levonorgestrel
- Ethinyloestradiol and levonorgestrel are metabolised by CYP3A4
- St John’s wort may induce CYP3A4
- St John’s wort may reduce ethinyloestradiol and levonorgestrel blood levels leading to breakthrough bleeding and reduced efficacy of the oral contraceptive
- Interaction is well documented, and pregnancies have occurred
- Patients should be counselled not to take St John’s wort if they are taking oral contraceptives

Why should Simvastatin not be taken with potent CYP3A4 inhibitors like erythromycin, itraconazole and ritonavir?
Pharmacokinetic Interactions
- Simvastatin must not be used with potent CYP3A4 inhibitors such as erythromycin, itraconazole and ritonavir
- If these medications must be used, simvastatin must be stopped for the duration of therapy
- Fatalities have occurred with combination therapy

Why should you avoid Grapefruit juice when taking Felodipine?
Pharmacokinetic Interactions
- Grapefruit juice contains compounds known as furanocoumarins that inhibit CYP3A4 and reduce the metabolism of felodipine leading to an increase in felodipine blood levels and possible flushing, hypotension and peripheral oedema (also Seville oranges and limes)
- Cigarette smoke may induce CYP1A1 and CYP1A2 leading to increased metabolism of caffeine, clozapine and olanzapine

What is Tamoxifen?
Which enzyme is responsible for its coversion to the active metabolite?
Tamoxifen
- Tamoxifen is a selective oestrogen receptor modulator (SERM)
- It is a pro-drug and is metabolised to 4 hydroxytamoxifen and 4 hydroxy-N- desmethyltamoxifen (endoxifen)
- Both metabolites are active, but endoxifen is thought to be most important for activity
- Exerts anti-oestrogenic activity in breast tissue, but oestrogenic activity on some other tissues e.g. the endometrium
- Tamoxifen is converted to endoxifen by CYP2D6
Why should Paroxetine be avoided when on Tamoxifen?
Tamoxifen & Paroxetine
- SSRI’s inhibit CYP2D6 to varying degrees
- Paroxetine is a very potent inhibitor of CYP2D6
- Paroxetine inhibits the conversion of tamoxifen to endoxifen = makes tamoxifen useless (takes out it’s anti-oestrogen effect)
- Paroxetine use during tamoxifen therapy has been reported in some studies to increase the risk of death from breast cancer

What is P-glycoprotein?
P-glycoprotein
- Is a carrier molecule (pump) which plays an important part in the absorption, distribution and elimination of some drugs
- It is an ATP-binding cassette (ABC) transporter (requires energy)
- It moves compounds out of cells (efflux transporter)
- Located in several tissues in the body including the kidneys, the gastrointestinal tract and the blood brain barrier
What are Functions of P-glycoprotein in the:
- Liver?
- Kidneys?
- Placenta?
- Intestine?
- Brain?
Functions of P-glycoprotein

What are some substrates, inhibitors and inducers of P-glycoprotein?

How is Digoxin absorbed/metabolised//excreted?
Digoxin
- Digoxin is not metabolised and is excreted as unchanged drug, primarily in the urine
- Digoxin is a substrate for P-glycoprotein
- P-glycoprotein in the gastrointestinal tract limits the absorption of digoxin → p-gycoprotein will limit digoxin absorption as it pumps it back into GIT
- P-glycoprotein in the renal tubules facilitates the renal elimination of digoxin
Why should Digoxin and Clarithromycin not be taken together?
Pharmacokinetic Interactions – Metabolism
Interaction Between Digoxin and Clarithromycin
- Digoxin is a substrate for P-glycoprotein
- If a P-glycoprotein inhibitor such as clarithromycin is taken together with digoxin the inhibition of P-glycoprotein by clarithromycin may lead to an increase in digoxin blood levels
- Inhibition of P-glycoprotein in the gut increases the absorption of digoxin
- Inhibition of P-glycoprotein in the kidney decreases the renal excretion of digoxin
- This may result in digoxin toxicity - e.g.nausea, confusion, bradycardia and cardiac dysrhythmias



