14.1 Eye disease Flashcards
(76 cards)
What is required for us to be able to see?
- Eye
- Clear cornea
- Clear lens
- Functioning retina and optic nerve
- Brain
- LGN (lateral geniculate nucleus)
- Superior colliculus
- Edinger-Westphal nucleus
- III nucleus
- IV nucleus
- VI nucleus
-
Frontal lobe (voluntary eye movements)
- Causes body movements
-
Vestibular nuclei
- Gaze stabilisation
-
Occipital lobe
- Pursuit eye movements & accomodation
- Dorsal stream (where it is?)
- Ventral stream (what it is?)
- CN III, IV, VI

What do different areas of the eye do?
- Cornea = refraction
- Lens = focussing
- Iris = controlling amount of light entering the eye
- Retina = phototransduction
- Optic nerve = carrying electrical signals to the brain

What is the function of the cornea & the layers?
- Main function is refraction
- 5 layers
- NO blood vessels but can grow but affect vision
- O2 (oxygen) from the atmosphere

What is normal refraction called and give examples of refractive errors and how to correct them?

What is astigmatism & explain it
- Cornea is not spherical
- Different radii of curvature in different axes
- In this case the vertical radius is shorter than the horizontal radius therefore the curvature of the cornea is steeper in the vertical axis than the horizontal axis.
- To correct this a cylindrical lens is needed with different powers in the different axes.
List some corneal diseases
- Corneal ulcer
- Corneal dystrophy
- Keratoconus
- Corneal oedema
What is this & explain it

CORNEAL ULCER
- Usually due to poor hygiene in contact lens wearers
- Can be treated with antibiotics
What is this?

Corneal dystrophy (rare)
What is this?

Keratoconus
- Treatment with corneal graft (given to allow good vision)
What is this?

Corneal oedema
- Due to failure of endothelial pumps
- Treatment with corneal graft
What is this?

Corneal graft
- Given to allow good vision
Explain what happens in the lens
- Some refraction
- Accommodation/fine focus:
- Circumferential ciliary muscle contracts allowing lens capsule to relax, lens becomes more spherical
- As we age this gets worse

What is cataract & what are the risk factors & treatment?
- Cataract: clouding of the lens
- Risk factors:
- Age
- Diabetes
- Corticosteroids
- Congenital
- Trauma
- Treatment
- Can be treated by surgery
What is this condition?
Cataracts
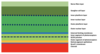
What are all the layers in the retina?
Inner at top
Outer at bottom (photoreceptors where transduction occurs)
What is the blood supply to the retina?
Blood from:
-
Central retinal artery
- Supplies innermost layers
-
Choroid artery
- Supplies outermost layers
What is the imaging of this picture?

Optical coherence tomography
What is the foveal dip?
- Where light entering the eye causes the sharpest image
- Increase in visual acuity
- Increase in determination of colour
-
Fovea appears slightly darker as it is thinnest here
- Choroid is most visible
- Hence, light can get straight to photoreceptors

What is the concentration of rods & cones in the retina?
-
RODS
- 6.5 million
- Increase numbers at the fovea
-
CONES
- 120 million
- None at fovea
- Widely spread throughout the retina
-
OPTIC DISC
- NO photoreceptors at the optic disc
Explain photoreceptors & the structure of them
- Photoreceptors is where phototransduction occurs
- Rods = scotopic vision (vision under LOW light levels)
- Cones = photopic vision (vision under WELL-lit conditions)
-
DISKS hold opsin molecules
- Rhodopsin in rods
- Iodopsin in cones
- Light stimulates the isomerisation of retinal which activates opsin leading to hyperpolarisation of the photoreceptor
-
3 different opsins present in all cones but one predominates in each of three different cones:
- “Blue” cones containing mostly blue-sensitive opsin are excited chiefly by a wavelength of around 420 nm,
- “Green” cones by a wavelength around 530 nm,
- “Red” cones by a wavelength near 560 nm

Explain phototransduction in detail

Role of ON-OFF switches in phototransduction
- Are to do with the modification of signal by transduction
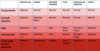
List some retinal diseases
- Colour blindness
- Retinal vascular occlusion
- Diabetes
- Macular degeneration
- Retinal detachment
Explain colour blindness & how it can be tested
- There are many forms of colour blindness
- Depends on which cones are affected (total loss/do not function properly)
- Red-Green colour blindness is the most common type
- Naming of colour blindness:
- Prot- = Red (L) cones
- Deuter- = Green (M) cones
- Trit- = Blue (S) cones
- -anomaly = malfunctioning
- -anopia = absent
- Tested
- Using the Ishihara test plates