15 - Chest Pain Flashcards
(36 cards)
What is the method of taking history for pain?

What are some causes of chest pain?
- Respiratory e.g pneumonia, pleurisy
- GI e.g reflux
- MSK e.g rib fracture and costochondritis
- Aortic dissection

How can you tell the difference between cardiac and pleuritic pain?

What will a patient history of chest pain due to the lungs/pleura present as?
- Pain more lateral than central
- Sharp pain, well localised, made worse by breathing in or coughing
What will a patient with chest pain due to MSK or the skin present as?
- Well localised
- Sharp
- Tender to palpate
- Well localised
e. g shingles or rib fracture
What will a patient with chest pain due to aortic dissection present as?
- Sharp tearing pain radiating into the back

What will a patient with chest pain due to heart tissue present as?
- Central not lateral pain
- Pain is dull or crushing
- Pain may radiate to jaw, shoulder, arms

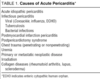
What is the typical history of pericarditis?
- Secondary to viral illness (recent cough)
- Retrosternal sharp chest pain localised to front of chest
- Aggravated with inspiration, cough, lying flat
- Eased by sitting up and leaning forward
- May hear pericardial rub
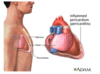
What would an ECG look like when someone has pericarditis?
Widespread saddle shaped ST elevation over a number of leads

What are the risk factors for atherosclerosis and what can it lead to?

What is the typical patient history of stable angina and why is this pattern of pain occurring?
- Pain on exertion, relieved by rest and GTN spray
- Cardiac chest pain that is dull and central
- Pain not severe
- Not associated with sweating and nausea

What disorders are included in acute coronary syndrome?
- Unstable angina
- MI: STEMI or NSTEMI
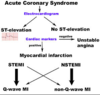
Why does acute coronary syndrome occur?
Atheromatous plaque ruptures and thrombus forms causing an acute increased occlusion and potential infarction

What would a patient’s history appear as if they have unstable angina and what is the risk of this syndrome?

How do you distinguish between UA, NSTEMI and a STEMI?
- ECG’s
- Blood tests

What would a patient’s history appear as with an MI?
- Sweating, nausea, vomiting
- No relieving factors
- Rising pulse
- Pain may radiate to neck, jaw, arms

What are the clinical examination findings of stable angina and acute coronary syndromes?

What would ECG changes look like in a STEMI?
or left bundle branch block

What would ECG changes look like in an unstable angina and NSTEMI?
ASSOCIATIED WITH ISCHAEMIA - use blood test to differentiate between the two

What are the different classifications of MI’s?

What questions do you have to answer when investigating ACS?
- What happened?
- When did it happen?
- Where did it happen?
- How bad is it?
- Why did it happen?
What investigations should you do into an ACS?
- Chest X-ray (pulmonary oedema)
- U and E (AKI)
- ECG and cardiac monitoring
- Echocardiogram (complications like mitral regurgitation)
- Invasive coronary angiogram
- FBC (anaemia)
- Lipid profile (triggers)

How do troponin levels change after an MI?
Starts to raise 3hrs after cardiac damage, peak at 24 to 48 hours, remains elevated for 2 weeks

What is an invasive coronary angiogram?
- Local anaesthetic
- Radial or femoral artery
- Option of dilating narrowed sections or including CT