12 - ECG Abnormalities Flashcards
(37 cards)
When are the PR, QRS and QT interval abnormal?

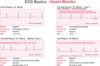
What are the three different types of heart block and explain what they look like on the ECG?
- 1st degree: longer PR
- Mobitz Type I/Wenkebach: Increasing PR and then drop of QRS
- Mobitz Type II: Normal PR and then random drop
- 3rd degree (complete block): P and QRS not linked with ventricular rate very slow
What are the causes of heart block?
- MI or degenerative changes
- Due to failure of conduction either from AV node, or Bundle of His

Why would a myocardial infarction lead to heart block?
Coronary artery occlusion in the right so no blood supplying the SAN etc
What is the issue with Type II Mobitz?
- High risk of progression to complete heart block
- Dangerous rhythm so need pacemaker to prevent this
How do you diagnose and treat 3rd degree heart block?
- Complete failure of atrioventricular conduction
- Ventricular escape rhythm so wide QRS
- Slow ventricular conduction rate
- Urgent pacemaker

What is bundle branch block?
- P wave and PR interval normal
- Wide QRS >3 small boxes as takes longer for depolarisation past delayed conduction in R or L bundle branches
WILLIAM MARROW

What are the two classifications of arrhythmias?

What will supraventricular and ventricular rhythms look like on an ECG?

What is atrial fibrillation and what would it appear as on the ECG?
- Supraventricular rhythm where rhythm comes from multiple atrial foci
- No P waves, wavy baseline
- Not all atrial are conducted as some in refractory period so irregular R-R and narrow QRS

What is a ventricular ectopic beat?
- Slower depolarisation so wide QRS as impulse not spreading down normal His-Purkinje system

What is ventricular tachycardia?
- Run of more than 3 ventricular ectopics
- Regular broad tachycardia
- Dangerous rhythm that needs urgent treatment as risk of VF

What is ventricular fibrillation?
- Abnormal irregular fast ventricular depolarastion
- Multiple ectopic sites so no co-ordinated contraction
- No cardiac output and cardiac arrest

How do you treat ventricular fibrillation and how does it work?
- Defibrillator as it is a shockable rhythm
- Puts all of the ventricular myocytes into repolarisation so they all depolarisation at the same time

What are the questions you should ask yourself when looking at an ECG?

Draw a tree diagram of the classifications of arrythmias?

By looking at an ECG how would you see which coronary artery there has been an occlusion in?

What is an acute STEMI?
- Complete occlusion of the coronary artery by thrombus and the full thickness of the myocardium is involved
- Sub-epicardium damage causes ST elevation in the leads facing the occlusion
- Need instant treatment to stop necrosis

How does a STEMI evolve on an ECG over time?
- Q wave due to necrosis so lead looks through the infarction to the other side so signal travelling away from it
- T-waves invert due to reversal of repolarisation

What is a pathological Q wave?
>1 small square wide
>2 small squares deep
Depth more than 1/4 of the height of following R wave

What does an old MI look like on an ECG?
Pathological Q waves as some areas of necrosis

What does a non-stemi ECG look like and why?
- Subendocardial injury leading to ST depression and/or T wave depression
- Cardiac ischaemia or infarction not affecting full thickness of the wall

How do you tell the difference between unstable angina (severe ischemia) and NSTEMI on an ECG?
Can’t tell a difference, have to differentiate using troponin as marker for muscle necrosis

What does stable angina look like on ECG?
- ST depression only occurs when exercising and reverses at rest
- Could have narrowed coronary artery










