Bones Flashcards
(51 cards)
Bones
Bone is specialised a type of connective tissue. It has a unique histological appearance, which enables it to carry out its numerous functions:
Haematopoeisis – the formation of blood cells from haematopoietic stem cells found in the bone marrow.
Lipid and mineral storage – bone is a reservoir holding adipose tissue within the bone marrow and calcium within the hydroxyapatite crystals.
Support – bones form the framework and shape of the body.
Protection – especially the axial skeleton which surrounds the major organs of the body.
Types of Bone Cells

Osteoblasts – Synthesises uncalcified/unmineralised ECM called osteoid. This will later become calcified/mineralised to become bone.
Osteocytes – As the osteoid mineralises, the osteoblasts become entombed between lamellae in lacunae where they mature into osteocytes. They then monitor the minerals and proteins to regulate bone mass.
Osteoclasts – Derived from monocytes and resorb bone by releasing H+ ions and lysosomal enzymes. They are large and multinucleated cells.
Structure of Bone
Under the microscope, bone can be divided into two types:
Woven bone (primary bone) – Appears in embryonic development and fracture repair, as it can be laid down rapidly. It consists of osteoid (unmineralised ECM), with the collagen fibres arranged randomly. It is a temporary structure, soon replaced by mature lamellar bone.
Lamellar bone (secondary bone) – The bone of the adult skeleton. It consist of highly organised sheets of mineralised osteoid. This organised structure makes it much stronger than woven bone. Lamella bone itself can be divided into two types – compact and spongy.
In both types of bone, the external surface is covered by a layer of connective tissue, known as the periosteum. A similar layer, the endosteum lines the cavities within bone (such as the medullary canal, Volkmann’s canal and spongy bone spaces).
Lamellar bone can be divided into two types. The outer is known as compact bone – this is dense and rigid. The inner layers of bone are marked by many interconnecting cavities, and is called spongy bone.
Compact Bone
Compact bone forms the outer ‘shell’ of bone. In this type of bone, the lamellae are organised into concentric circles, which surround a vertical Haversian canal (which transmits small neurovascular and lymphatic vessels). This entire structure is called an osteon, and is the functional unit of bone.
The Haversian canals are connected by horizontal Volkmann’s canals – these contain small vessels that anastamose (join together) the arteries of the Haverisan canals.
Osteocytes are located between the lamellae, within small cavities (known as lacunae). The lacunae are interconnected by a series of interconnecting tunnels, called canaliculi.
Spongy Bone

Spongy bone makes up the interior of most bones, and is located deep to the compact bone. It contains many large spaces – this gives it a honeycombed appearance.
The bony matrix consists of a 3D network of fine columns, which crosslink to form irregulartrabeculae. This produces a light, porous bone, that is strong against multidirectional lines of force. The lightness afforded to spongy bone is crucial in allowing the body to move. If the only type of bone was compact, they would be too heavy to mobilise.
The spaces between trabeculae are often filled with bone marrow. Yellow bone marrow refers to adipocytes and red bone marrow consists of haematopoietic stem cells.
This type of bone does not contain any Volkmann’s or Haversian canals.
Embryonic Development of Bones
Ossification is the term for the formation of bone. There are two ways that bone can ossify during embryonic development. Each way has its own name: intramembranous ossification and endochondral ossification. Because of these two ways that bone can develop, two types of bone can be described to exist based on the way they developed embryonically: intramembranous bones and endochondral bones. The intramembranous bones are always flat bones, but the endochondral bones include the long, short, and irregular bones.
Growth of Bones

Long bones lengthen at the epiphyseal plate with the addition of bone tissue and increase in width by a process called appositional growth.
The epiphyseal plate, the area of growth composed of four zones, is where cartilage is formed on the epiphyseal side while cartilage is ossified on the diaphyseal side, thereby lengthening the bone.
Each of the four zones has a role in the proliferation, maturation, and calcification of bone cells that are added to the diaphysis.
The longitudinal growth of long bones continues until early adulthood at which time the chondrocytes in the epiphyseal plate stop proliferating and the epiphyseal plate transforms into the epiphyseal line as bone replaces the cartilage.
Bones can increase in diameter even after longitudinal growth has stopped.
Appositional growth is the process by which old bone that lines the medullary cavity is reabsorbed and new bone tissue is grown beneath the periosteum, increasing bone diameter.
Vertebral Column

The most important functions of the vertebral column are as follows:
Protection: it encloses the spinal cord, shielding it from damage.
Support: it carries the weight of the body above the pelvis (below the pelvis, the lower limbs take over).
Axis: the vertebral column forms the central axis of the body.
Movement: it has roles in both posture and movement.
The vertebral column can be separated into five different regions. Each region is characterised by a different vertebral structure. Before looking, at individual structures, we first need to look at the general form of a vertebra.

Vertebral Structure
Although vertebrae do have significant differences in size and shape between groups, they have the same basic structure. Each vertebrae consists of avertebral body, situated anteriorly, and a posterior vertebral arch.
Pedicles: There are two of these, one left and one right. They point posteriorly, meeting the flatter laminae.
Lamina: The bone between the transverse and spinal processes.
Transverse processes: These extend laterally and posteriorly away from the pedicles. In the thoracic vertebrae, the transverse processes articulate with the ribs.
Articular processes: At the junction of the lamina and the pedicles, superior and inferior processes arise. These articulate with the articular processes of the vertebrae above and below.
Spinous processes: Posterior and inferior projection of bone, a site of attachment for muscles and ligaments.

Cervical Vertebrae

There are seven cervical vertebrae in the human body. They have three main distinguishing features:
The spinous process bifurcates into two parts, and so is known as a bifid spinous process.
There are two transverse foramina, one in each transverse process. These conduct the vertebral arteries.
The vertebral foramen is triangular in shape
There are some cervical vertebrae that are unique. C1 and C2 (called the atlas and axis respectively), are specialised to allow for the movement of the head.
The C7 vertebrae has a much longer spinous process, which does not bifurcate.
Thoracic Vertebrae

The twelve thoracic vertebrae are medium sized, and increase in size as they move down the back. Their main function is to articulate with ribs, producing the bony thorax.
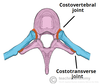
Each thoracic vertebrae has two ‘demi facets‘ on each side of its vertebral body. These articulate with the head of the respective rib, and the rib inferior to it. On the transverse processes of the thoracic vertebrae there is a costal facet for articulation with its respective rib.
The spinous processes are slanted inferiorly and anteriorly. This offers increased protection to the spinal cord, preventing an object like a knife entering the spinal canal through the intervetebral discs.
In contrast to the cervical vertebrae, the vertebral foramen is circular.
Lumbar Vertebrae
These are the largest of the vertebrae, of which there are five. They act to support the weight of the upper body, and have various specialisations to enable them do this.
Lumbar vertebrae have very large vertebral bodies, which are kidney shaped. They lack the characteristic features of other vertebrae, with no foramen transversarium, costal facets, or bifid spinous processes.
However, like the cervical vertebral, they have a triangular shaped vertebral foramen.
Sacrum and Coccyx
The sacrum is a collection of five fusedvertebrae. It is described as a upside downtriangle, with the apex pointing inferiorly. On the lateral walls of the sacrum are facets, for articulation with the pelvis at the sacro-iliac joints.
The coccyx is a small bone, which articulates with the apex of the sacrum. It is recognised by its lack of vertebral arches. Due to the lack of vertebral arches, there is no vertebral canal, and so the coccyx does not transmit the spinal cord.

Vertebral Joints
For every vertebrae, there are five articulations. The vertebral bodies indirectly articulate with each other, and the articular processes also form joints.
The vertebral body joints are cartilaginous joints, designed for weight bearing. The articular surfaces are covered by hyaline cartilage, and are connected by a fibrocartilage intervertebral disk. There are two ligaments that strengthen these joints; the anterior and posteriorlongitudinal ligaments. The anterior longitudinal ligament is thick and prevents hyperextension of the vertebral column. The posterior longitudinal ligament is weaker and prevents hyperflexion.
The joints between the articular facets are called facet joints. These allow for some gliding motions between the vertebrae. They are strengthened by various ligaments:
Ligamentum Flavum: extends from lamina to lamina.
Interspinous and Supraspinous ligaments: These join the spinous processes together. The interspinous ligaments attach between processes, and the supraspinous ligaments attach to the tips.
Intertransverse ligaments: extends between transverse processes.
Hip Bone

The hip bones have three articulations:
Sacroiliac joint – articulation with sacrum.
Pubic symphysis – articulation with the corresponding hip bone.
Hip joint – articulation with the head of femur.
The hip bone is made up of the three parts – the ilium, pubis and ischium. Prior to puberty, the triradiate cartilage separates these constituents. At the age of 15-17, the three parts begin to fuse.
Their fusion forms a cup-shaped socket known as the acetabulum, which becomes complete at 20-25 years of age. The head of the femurarticulates with the acetabulum to form the hip joint.
Ilium

The superior part of the hip bone is formed by theilium, the widest and largest of the three parts. The body of the ilium forms the superior part of theacetabulum. Immediately above the acetabulum, the ilium expands to form the wing (or ala).
The wing of the ilium has two surfaces. The inner surface is concave, and known as the iliac fossa, providing origin to the iliacus muscle. The external surface is convex, and provides attachments to the gluteal muscles. Hence it is known as the gluteal surface.
The superior margin of the wing is thickened, forming the iliac crest. It extends from the anterior superior iliac spine to the posterior superior iliac spine.
Muscles attaching to the Ilium: –
Gluteal muscles attach to the external surface of the Ilium at the anterior, posterior and inferior gluteal lines.
The iliacus muscle attaches medially at the iliac fossa.

Pubis

The pubis is the most anterior portion of the hip bone. It consists of a body and superior and inferior rami (branches).
The body is located medially, articulating with its opposite pubic body, at the pubic symphysis.
The superior rami extends laterally from the body, forming part of the acetabulum. The inferior rami projects towards, and joins the ischium. Together, the two rami enclose part of the obturator foramen, through which the obturator nerve, artery and vein pass through to reach the lower limb.
Ischium

The posterioinferior part of the hip bone is formed by the ischium. Much like the pubis, it is composed of a body, an inferior and a superior ramus.
The inferior ischial ramus combines with the inferior pubic ramus forming the ischiopubic ramus which encloses part of the obturator foramen. The posterorinferior aspect of the ischium forms the ischial tuberosities and when sitting, it is these tuberosities on which our body weight falls.
On the posterior aspect of the ischium there is an indentation known as the greater sciatic notch, with the ischial spine at its most inferior edge.
The important ligaments attach to the ischium:
The sacrospinous ligament runs from the the ischial spine to the sacrum, thus creating the greater sciatic foramen through which lower limb neurovasculature (including the sciatic nerve) and the piriformis muscle transends.
The sacrospinous ligament and thesacrotuberous ligament run from the sacrum to the ischial tuberosity, forming the lesser sciatic foramen.
Joints
A joint is defined as the point at which two or more bones make contact (or articulate). In this article we shall look at the structure and classification of different types of joints.
Joints can be classified by the type of tissue present. Using this method, we can split the joints of the body into fibrous, cartilaginous and synovial joints.
Fibrous Joints

A fibrous joint is where the bones concerned are bound by fibrous tissue. Fibrous joints can further subclassified into sutures, gomphmoses and syndesmoses.
Sutures
Immovable joint (called a synarthrosis)
Only found between the bones of the skull.
There is limited movement until about 20 years of age, after which they become fixed.
Gomphmoses
Immovable joint (called a synarthrosis) Where the teeth articulate with their sockets in the maxillae (upper teeth) or the mandible(lower teeth) The fibrous connection that binds the tooth and socket is the periodontal ligament
Syndesmoses
Slightly movable joins (called an amphiarthrosis)
Usual structure is bones held together by together by an interosseous membrane
Middle radio-ulnar and middle tibiofibular joint are key examples
Cartilaginous Joints

In cartilaginous joints, the bones are attached by fibrocartilage or hyaline cartilage. They be split into primary and secondary cartilgainous joints.
Synchondroses
Also known as primary cartilaginous joints, they only involve hyaline cartilage.
The joints can be immovable (synarthroses) or slightly movable (amphiarthroses)
The joint between the diaphysis and epiphysis of a growing long bone is asynchondrosis. This is interesting in that it is a temporary joint with no movement.
Symphyses
Also known as a secondary cartilaginous joint, it can involve fibrocartilage or hyaline cartilage
The joints are slightly movable (amphiarthroses)
An example of a symphysis is the pubic symphysis.
Synovial Joints

A synovial joint is a joint filled with synovial fluid. These joints tend to be fully moveable (known as diarthroses), and are the main type of joint found around the body. They are defined by the arrangement of their articular surfaces, and types of movement they allow.
Hinge
Permits flexion and extension
Elbow joint is a notable example
Saddle
Concave and convex joint surfaces
E.g. Metatarsophalangeal joint
Plane
Permit gliding or sliding movements
E.g. Acromioclavicular joint
Pivot
Allows rotation; a round bony process fits into a bony ligamentous socket
E.g. Atlantoaxial joint & proximal radio-ulnar joint
Condyloid
Permits flexion & extension, adduction, abduction & circumduction
E.g. Metacarpophalangeal joint
Ball & Socket
Permits movement in several axis; a rounded head fits into a concavity
E.g. Glenohumeral Joint.
Ribs

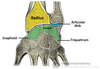
The typical rib consists of a head, neck and body:
The head is wedge shaped, and has two articular facets separated by a wedge of bone. One facet articulates with the numerically corresponding vertebrae, and the other articulates with the vertebrae above.
The neck contains no bony prominences, but simply connects the head with the body. Where the neck meets the body there is a roughed tubercle, with a facet for articulation with the transverse process of the corresponding vertebrae.
The body, or shaft of the rib is flat and curved. The internal surface of the shaft has a groove for the neurovascular supply of the thorax, protecting the vessels and nerves from damage.

Atypical Ribs
Ribs 1, 2, 11 and 12 can be describes as ‘atypical’ – they have features that are not common to all the ribs.
Rib 1 is shorter and wider than the other ribs. It only has one facet on its head for articulation with its corresponding vertebrae (there isn’t a thoracic vertebrae above it). The superior surface is marked by two grooves, which make way for the subclavian vessels.
Rib 2 is thinner and longer than rib 1, and has two articular facets on the head as normal. It has a roughened area on its upper surface, where the serratus anterior muscle attaches.
Ribs 11 and 12 have no neck, and only contain one facet, which is for articulation with the corresponding vertebrae.