10/14- Large Intestine, Pathology Flashcards
T/F: There are villi and crypts in the colon
False
- Colon has crypts but no villi
- Crypts look like racked test tubes and reach muscularis mucosa

What is seen here?

Cross section of previous pic
- Crypts are equally spaced with mild lymphoplasmacytic infiltrate and capillaries
Describe Entamoeba histolytica
- Transmission
- Prevalence
- Characteristics of agent
- Reproduction
- Location
- Disease
- Amebiasis
- Fecal-oral transmission
- Esp developing countries (500M)
- E. histolytica cysts has a chitin wall and four nuclei
- Resistant to gastric acid: pass through the stomach
- Cysts colonize the epithelial surface of the colon and release trophozoites
- Most frequently in cecum and ascending colon
Results in:
- Dysentery
- Liver abscess
How does Entamoeba histolytica cause dysentery?
- Amebae attach to the colonic epithelium… apoptosis
- Invade crypts and burrow into lamina propria
- Neutrophils -> tissue damage
- Flask-shaped ulcer
How to identify Entamoeba histolytica histologially?
May be difficult; amebae are similar to macrophages
How does Entamoeba histolytica cause liver abscess?
- Parasites may penetrate splanchnic vessels
- Embolize to liver -> abscesses (40% of patients with amebic dysentery)
What is seen here?

Scanning EM of intestinal amebiasis
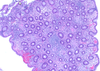
What is seen here?

Intestinal specimen from pt with acute amebic colitis
What is seen here?
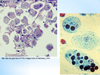
Entamoeba histolytica cause liver abscess?
What is the clinical presentation of Entamoeba histolytica?
- Abdominal pain, bloody diarrhea and weight loss
- Occasionally, acute necrotizing colitis and megacolon
- Significant mortality
How to treat Entamoeba histolytica?
(Obligate fermenters of glucose)
The most effective treatment: metronidazole
- Inhibits enzyme pyruvate oxidoreductase
What is Pseudomembranous colitis?
What commonly causes it?
Antibiotic-associated colitis or antibiotic-associated diarrhea
- Diarrhea during or after a course of antibiotic therapy
- Usually caused by Clostridium difficile
- Salmonella, C. perfringens type A
- Staphylococcus aureus
Describe the pathogenesis of Pseudomembranous colitis
- Disruption of the normal colonic flora by antibiotics allows C. difficile overgrowth
- Most commonly: third-generation cephalosporins
- Predisposing factor: immunosuppression
- Toxins:
- Ribosylation of small GTPases, such as Rho
- Disruption of the epithelial cytoskeleton, tight junction barrier loss, cytokine release and apoptosis
What are risk factors for Pseudomembranous colitis?
- Advanced age
- Hospitalization
- Antibiotic treatment
Up to 30% of hospitalized adults are colonized with C. difficile (tenfold greater than the general population)
What is seen here?

Psuedomembranes (C. difficile) in Pseudomembranous colitis
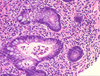
What is seen here?

Pseudomembranous colitis
- “Volcano eruption” of neutrophils and dead cells is common
- Increased chronic inflammatory cells in lamina propria

What is seen here?

Pseudomembranous colitis
- Higher magnification of volcano eruption of neutrophils and dead cells
What is the clinical presentation of Pseudomembranous colitis?
How is it diagnosed?
- Fever, leukocytosis
- Abdominal pain, cramps,
- Hypoalbuminemia
- Watery diarrhea and dehydration
+/- fecal leukocytes and occult blood
Diagnosis: C. difficile toxin and characteristic histopathology
Treatment for Pseudomembranous colitis (C. difficile)?
- Metronidazole
- Vancomycin
What is Inflammatory bowel disease?
What does it include? (Important!)
Chronic condition due to inappropriate mucosal immune activation
Two disorders: Crohn disease and ulcerative colitis
- Ulcerative colitis: a severe ulcerating inflammatory disease limited to colon and rectum involving mucosa and submucosa
- Crohn disease: regional enteritis, involves any area of the GI tract and typically transmural
Pictoral difference between Crohn’s disease and ulcerative colitis? (Important!)
Crohn’s:
- Skip lesions (not continuous)
- Transumural inflammation,ulcerations, fissures
Ulcerative colitis:
- Continuous colonic involvement beginning in the rectum
- Pseudopolyps and ulcers

Describe the epidemiology of IBD
- More in females
- Common in teens/early 20s
- Most common in Caucasians in Western industrialized nations
- 3-5x more in eastern European (Ashkenazi) Jews
- Geographic distribution is highly variable
- Most common in N America, N Europe, and Australia
Pathogenesis of IBD (picture)

Describe the pathogenesis of IBD
In genetically susceptible host, release of TNF and other immune-mediated signals epithelia
- > increase tight junction permeability
- > further increases in the flux of luminal material
- Self-amplifying cycle to initiate
A variety of factors are associated with disease for unknown reasons
- Appendicitis: reduced risk of developing UC
- Tobacco modifies IBD epidemiology: increase risk of Crohn while reduce risk of UC