S4) The Leg Flashcards
What is the tibia?
The tibia is the main bone of the leg, expanding at the proximal and distal ends and articulating with the knee and ankle joints respectively

Describe the features of the proximal end of the tiba
- Medial and lateral condyles (form the tibial plateau)
- Intercondylar eminence (two tubercles & a roughened area)
- Tibial tuberosity (anterior surface)

Describe the proximal articulations of the tibia with the femur
- Medial and lateral condyles articulate with condyles of femur
- Tibial intercondylar tubercles fit into the intercondylar fossa of the femur

Describe the posterior surface of the shaft of the tibia.
- Marked by a ridge of bone called the soleal line which runs inferomedially, blending with the medial border of the tibia
- Marked by a groove where the tibialis posterior muscle attaches

Describe the features of the anterior and lateral borders of the shaft of the tibia
- Anterior border – marked by tibial tuberosity
- Lateral border (aka interosseous border) – attachment site for interosseous membrane which binds the tibia and fibula

Describe the features of the distal region of the tibia
- Medial malleolus – bony projection continuing inferiorly & articulates with the tarsal bones to form part of the ankle joint
- Fibular notch – found laterally, where the fibula is bound to the tibia

What is the fibula?
The fibula is a thin bone of the leg found laterally to the tibia and does not articulate with the femur at the knee joint but rather acts as an attachment for muscles

Describe the features of the distal and proximal ends of the fibula
- Proximal: enlarged head with a facet for articulation with the lateral condyle of the tibia
- Distal: lateral surface continues inferiorly producing a bony projection (lateral malleolus - more prominent)

Identify the four muscles in the anterior compartment of the leg
- Tibialis anterior
- Extensor digitorum longus
- Extensor hallucis longus
- Fibularis tertius
Describe the neurovascular supply of the anterior compartment of the leg
- Arterial supply via the anterior tibial artery
- Innervation via deep fibular nerve

Describe the anatomical location and function of the tibialis anterior muscle

- Location: located on lateral surface of tibia
- Function: dorsiflexion, inversion

State the origin and attachment of the tibialis anterior muscle

- Origin: lateral surface of the tibia
- Attachment: medial cuneiform and base of metatarsal I

Describe the anatomical location and function of the extensor digitorum longus muscle

- Location: lies lateral and deep to the tibialis anterior
- Function: dorsiflexion, extension of the lateral four toes

State the origin and attachment of the extensor digitorum longus muscle

- Origin: lateral condyle of tibia and medial surface of fibula
- Attachment: tendon splits into four, each inserting onto a toe

Describe the anatomical location and function of the extensor hallucis longus

- Location: deep to the extensor digitorum longus and tibialis anterior
- Function: great toe extension, dorsiflexion

State the origin and attachment of extensor hallucis longus

- Origin: medial surface of the fibular shaft
- Attachment: base of the distal phalanx of the great toe

Describe the anatomical location and function of the fibularis tertius muscle

- Location: arises from the most inferior part of the extensor digitorum longus (not present in all individuals)
- Function: eversion, dorsiflexion

State the origin and attachment of the fibularis tertius muscle

- Origin: medial surface of the fibula
- Attachment: metatarsal V (diverges from EDL at dorsum of foot)

Identify the two muscles in the lateral compartment of the leg
- Fibularis longus
- Fibularis brevis

Describe the structure, function and innervation of the fibularis longus muscle
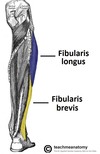
- Structure: larger and more superficial muscle within the compartment
- Function: plantarflexion, eversion, supports the lateral and transverse foot arches
- Innervation: Superficial fibular nerve

State the origin and attachment of the fibularis longus muscle

- Origin: superior and lateral surface of fibula and lateral tibial condyle (moves posterior to the lateral malleolus)
- Attachment: medial cuneiform and base of metatarsal I (crosses under foot)

Describe the structure, function and innervation of the fibularis brevis muscle

- Structure: deeper and shorter than fibularis longus
- Function: eversion
- Innervation: superficial fibular nerve

State the origin and attachment of the fibularis brevis muscle

- Origin: inferolateral surface of the fibular shaft (travels posteriorly to the lateral malleolus)
- Attachment: tubercle on metatarsal V (past over calcaneus and cuboid)

Identify the two types of muscles in the posterior compartment of the leg
- Superficial muscles
- Deep muscles
The two layers are separated by a band of fascia
The superficial muscles of the posterior leg all insert into the calcaneus of the foot via the calcaneal tendon.
Identify and describe the two bursae associated with the calcaneal tendon
- Subcutaneous calcaneal bursa – lies between the skin and the tendon
- Retrocalcaneal bursa – lies between the tendon and the calcaneus

Identify the superficial muscles of the posterior leg
- Soleus
- Gastrocnemius
- Plantaris
Describe the structure, function and innervation of the gastrocnemius muscle

- Structure: most superficial muscle in posterior leg, two heads – medial and lateral
- Function: knee flexion, plantarflexion
- Innervation: tibial nerve

State the origin and attachment of the gastrocnemius muscle

- Origin: lateral femoral condyle and medial femoral condyle
- Attachment: calcaneus

Describe the structure, function and innervation of the plantaris muscle

- Structure: small muscle with a long tendon (absent in 10% of people)
- Function: plantarflexion, knee flexion
- Innervation: tibial nerve

State the origin and attachment of the plantaris muscle

- Origin: lateral supracondylar line of the femur
- Attachment: blends with calcaneal tendon

Describe the structure, function and innervation of the soleus muscle

- Structure: large, flat, deep to the gastrocnemius
- Function: plantarflexion
- Innervation: tibial nerve


























































