80 + 81 Pediatric Neurology Flashcards
(53 cards)
1
Q
Amblyopia
- What is this?
- Can it be corrected right away?
A

2
Q
Amblyopia
- What are the 3 causes of unilateral Amblyopia?
A

3
Q
Amblyopia
- How is this usually corrected?
A

4
Q
Amblyopia
- When is the sensitivity period for Amblyopia?
- What does this suggest about vidual improvement?
- How common is this in North America?
A

5
Q
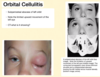
What is this?

A
Orbital Cellulitis
6
Q
Amblyopia
- What is used to detect Amblyopia?
A

7
Q
What is this?

A
Strabismus
8
Q
Strabismus
- What is this defined as?
- What is horizontal strabismus called?
- What is vertical strabismus called?
- What is it the leading cause of?
A

9
Q
Strabismus
- Exotropia
- Is this an outward or inward turning of the eye?
- When does it usually occur?
A

10
Q
Strabismus
- How common is this in the US?
- What is accommodative esotropia?
- How common is this?
A

11
Q
Pseudostrabismus
- What are the 2 reasons that children can have this?
A

12
Q
What is this?

A
Orbital Cellulitis
13
Q
- What is this?
- What would a CT show?

A
14
Q
Potts Puffy Tumor
- What is this defined as?
- What will a CT show?
A

15
Q
Migraines
- Who gets this more; males or females?
- What is a prodrome?
- When does it occur?
- What is an aura?
- What do the pateints experience?
- What are the red flags?
A

16
Q
Migraines
- How do you treat this?
A

17
Q
Brain tumors in children
- How common is this?
- How common is death?
- What is the most common type?
A

18
Q
Brain tumors in children
- How do these clinically manifest? (3)
A

19
Q
Brain tumors in children
- What is the triad?
- What is torticollis?
- How does this affect gait? Vision?
A

20
Q
Febrile Seizures
- What will patients have?
- What will they NOT have?
- When do most of these occur? (age, time related to fever)
- What will some patients have a history of?
- What are the risk factors for this? (4)
- What is the prognosis like?
A
21
Q
Febrile Seizure
- Differentiate between simple and complex?
- How will a complex febrile seizure present?
- How often does recurrence before the age of 6?
- How does epilepsy relate to this?
- What can cause the fever (6)
A

22
Q
Febrile Seizures
- What is NOT indicated in the treatment for this?
- How does acetaminophen and ibuprofen use relate to the treatment of this?
A
23
Q
Infantile Botulism
- What does the toxin inhibit?
- When is this most common in life?
- What history do patients usually have?
- What are the manifestations of this?
- What kind of paralysis occurs?
A
24
Q
Infantile Botulism
- Are these bacteria gram negative or positive?
- How long is the incubation period?
- Where in the US is this most common?
A

25
Non Accidental Trauma
* What are the 6 radiologic red flags?
26
Non Accidental Trauma
* What age will children start to have tru-self imposed injurtes?

27
Non Accidental Trauma
* Shaken Baby Syndrome (Abusive Head Trauma)
* What kind of hemorrhages occurs?
* How often does this Shaken Baby Syndrome in child abuse cases?
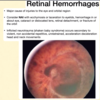
28
Non Accidental Trauma
* What is this?
* What do you consider NAT with it?

29
Tourette Disorder
* What are the 4 things that a Dx for Tourette Disorder?

30
Tic Disorders
* What are the criteria for Persistent (chronic) Tic Disorders? (5)
* What do you need to specify?

31
Tic Disorders
* What disorders may have tics in them?

32
Tic Disorders
* What is the criteria for provisional Tic Disorders? (5)

33
Tic Disorders
* Differentiate between simple motor and complex motor tics?
* What can trigger tics?
* What should be on your differential dx when considering if a patient has Tic Disorders?

34
Tics and Tourrettes
* Clinical Course
* When do patients get this? (Boys, Girls, PEak severity)
* Differentiate between simple vocal and complex vocal tics?
* Why do we think patients have tics?

35
Partial Arousal Parasomnias
* What happens to these patients?
* When does it occur in life?
* When do symptoms occur at night?
* Why may patients have this?
* How can patients help children who have this?
* What medications are used when this becomes serious?

36
Breath-Holding Spells
* What should parents do?
* What can this lead to?

37
Sydenham Chorea
* What is another name for this?
* What condition occurs with about 10 to 20% of cases?
* When usually occurs about a month before this?
* What sex is affected most?
* What age?
* What history can a patient have?
* What part of the brain is affected?

38
What is this?
What can it cause?


39
Sydenham Chorea
* What are the clinical hallmarks of this? (3)
* What can help confirm an acute strep infection?
* Can this exclude the Dx?
* What do you give for longterm antibiotic prophylaxis?

40
Sydenham Chorea
* What is used because if its anti-dopamine effects?
* What ADR does this have?
* What medications are used to control movements?
* What immunomodulatory interventions occur?

41
Guillain-Barre Syndrome
* What is this?
* Is it mainly motor or sensory?
* Who does this effect?
* What cells are affected?
* What happens before paralysis sets in?
* What bacteria in the GI tract can cause this?
* The respiratory tract?
* What food can cause this?
* What are the viral causes of this?
* What vaccines are associated with this?

42
Guillain-Barre Syndrome
* What are the inital symptoms?
* Where does weakness begin?
* What kind of paralysis occurs?
* What mood are the children who have this in?

43
Neurofibromatosis
* Type 1
* What appears on the skin of these patients?

44
Neurofibromatosis
* Type 1
* What complications arise from this?

45
Tay Sachs Sialidosis
* What group of people get this?
* What gene/enzyme is affected?
* When do patients get this?
* How do they present?
* What is seen in the eyes of patients?

46
Sturge-Weber Syndrome
* What gene is implicated?
* What kind of vascular growth occurs?
* When do seizures occur?
* Relative the port wine birthmark
* What part of the brain is affected?
* Where do convulsions occur?
* Where does hemiparesis occur?

47
Sturge-Weber Syndrome
* Type 1
* How common is this?
* What kind of angiomas occurs?
* What happens to the eyes?
* When do seizures occur?
* What happens to the cognitive/physical development?

48
Sturge-Weber Syndrome
* Type 2
* What kind of angioma is seen?
* What happens to the eye?
* What is NOT seen?

49
Sturge-Weber Syndrome
* Type 3
* What kind of angioma is seen?
* What is NOT seen?
* How do you ID this?

50
Define these types of cerebral palsy


51
Spastic Cerebral Palsy
* What is affected spastic CP?
* How common is this?

52
Cerebral Palsy
* Dyskinetic CP
* What happens in this?
* Ataxic CP
* What happens in this?
* Causes of CP? (5)

53
Cerebral Palsy
* What are the risk factors?
* What are the signs and symptoms?



