Diagnostic Methods and Cycle Manipulation in the Mare Flashcards
- 4 days post covering you are asked to examine a mare because she has an itchy vulva
- Describe the lesions you see
- What is the possible cause and what are the consequences and actions you should take?

- Multiple Equine HV. 3 predominately causing these pustules which erode.
- Transmitted venereally
- See variety of adhesions as they age
- Start as these vesicular lesions which can burst and erode
- Mare will be sore and itchy
- Lesions would be on stallion too
- Transmission can be by stud and contamination of handler or material
- This mare will be shedding virus
- Actions: Isolate, don’t contaminate material, do not breed
- Consequence – this local disease (doesn’t cause pregnancy failure)
- If you are breeding – ensure no lesions at the time
What is the common diagnostic approach to a breeding exam?
- History
- Previous fertility
- Consider venereal pathogens
- General clinical examination
–Is she actually in oestrus or is she just showing odd signs?
- Mammary
- Perineum
- Vulva, vestibule, vagina, cervix
- Uterine palpation and ultrasound
- Ovarian palpation and ultrasound
What information do we need in a breeding exam relating to the history? (7)
•Current Presentation
–Pregnant
–With a foal at foot
–Barren (in equine terms meaning bred last year but did not get pregnant (just referring to last year))
–With a specific problem
•Really important questions are:
–Age of mare
–Previous breeding history
- Not pregnant
- Early pregnancy loss – did it establish? Maintained to full term?
- Abortion / stillbirth
- Need to establish if the mare can carry the pregnancy all the way through
–If barren
- What was the management last year?
- Who was the Vet last year?
- Number of years barren?
What do you look for on a general physical exam of a breeding mare?
- Body condition
- General observations
–Is she lame?
–Is she hairy?
- Feet
- Udder
What specific details do we need to know about the perineum? (7)
- Long axis of the vulval should be vertical
- Vulvar labia should be well apposed
- No vulval discharge
- No vulval lesions
- Perineum should be intact
- Anus should not be recessed
- Normal vestibulo-vaginal seal
–Need to part vulval lips to establish this
What can be seen on the images?

A) Normal
B) Sunken anus – cranially which causes vaginal sloping = increased faeces contamination and wind sucking
C) Palpating pelvis
D) Vestibulo-vaginal seal – ring structure (open). Risk of gas aspiration into vagina. Predisposed to cervixitits
E) Coital exanthema
What can the HBLB codes of practice give us guidance on? (8)
- Venereal transmitted bacterial diseases caused by the contagious equine metritis organism CEMO, Klebsiella pneumoniae and Pseudomonas aeruginosa
- Equine Viral Arteritis - EVA
- Equine Herpesvirus - EHV
- Equine Coital Exanthema - ECE
- Equine Infectious Anaemia - EIA
- Dourine
- Strangles
- Artificial Insemination – AI
What is the HBLB?
•What they do.. specific guidelines (not a law or absolute, just the best thing to do) each year for specific categories of mare (walk in, resident etc) for:
–Taylorella equigenitalia (Contagious equine metritis organism [CEMO])
–Klebsiella pneumoniae (Capsule types 1,2,5)
–Pseudomonas aeruginosa (specific strains but not possible to type these in routine testing so all are therefore [incorrectly] assumed to be pathogenic)
These define number of swabs, where from and how may repeats
How do you swab for bacterial veneral pathogens?
–You need to swab the fossa and sinus
(and in some cases the uterus)
–You need Amies transport media (e.g. charcoal)
•Taylorella is a microphillic
–You need to send to Approved Lab
–Culture needs to commence within 48h
What is seen in these images?

Left - Fossa
Middle - Sinus
Right -
Sinus smegma
Squeezing clitoris and see the waxy material (smegma). This is what we are swabbing. Organisms live.
What are the bacterial venereal pathogens we swab for? (5)
Discuss the different isolates for 2 of the bacteria
•Certificates simply state:
–Taylorella equigenitalia .. was / was not isolated
–Klebsiella pneumoniae .. was / was not isolated
–Pseudomonas aeruginosa.. was / was not isolated
- A separate section may indicate for Klebsiella what the capsule type was (remember capsule types 1,2,5 are the only ones that are pathogenic). Many types where some are venereal and some are not. The lab can easily differentiate this. E.g. if you had capsule 13 it wouldn’t stop you breeding.
- There will be no designation for strain of Pseudomonas. Some which are known venereal and some are environmental contaminants. Two sorts pathogenic and not – we cannot isolate which one we have.
What is the action if contagious equine metritis is isolated?
1. In mares prior to covering
- Stallions prior to covering
- Mares and stallions after covering
•In mares prior to covering
–Isolate and treat infected mares
–Notify owners of mares
•Stallions prior to covering
–Isolate and treat
–Notify owners of mares
•Mares and stallions after covering
–Cease covering
–Check all mares implicated in the outbreak
–Do not cover until 3 negative swabs each at least 2 days apart
What do mares need to be serologically negative to?
•Normally ensure mare is serologically negative to Equine Viral Arteritis (or vaccinated for this)
N.B. EVA is notifiable by law in the UK
How is EVA transmitted? (2)
•Transmitted both via respiratory tract route and also venereally (including chilled semen)
What are the signs of EVA? (4)
•Classic disease is flu-like but with significant conjunctivitis, (pink eye) focal dermatitis, limb and ventral oedema
What is the effect of EVA on pregannt mares?
- Pregnant mares that get infected may abort (abortion may relate to degree of immunity or pathogenicity of virus strain)
- Aborted fetuses appear partialy autolysed (unlike fresh fetuses in EHV) however still need appropriate pathological examination
When is EHV 1 vaccinated for?
planned for month 5, 7 and 9 of pregnancy e.g. Equip EHV 1,4
What do horses returning to the UK need to be serologically negative for?
EIA
Why do we undertake uterine swabs?
•Undertaken for bacterial venereal pathogen screening – we will do this based on previous history ; high or low risk. High risk – likely to have had a venereal pathogen previously so is recommended to uterine swab.
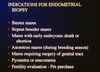
Why are uterine swabs undertaken? (3)
Endometritis:
–For endometrial cytology as part of detection of endometritis
–For endometrial bacteriology in cases of endometritis to ensure appropriate antimicrobial selection
–For the detection of other pathogens (yeast / fungi – requires specific culture medium)
When should we undertake a uterine swab?
•Uterine swabs are often taken during oestrus (this is HBLB guidance): but we will talk more about this later since probably collection in the luteal phase would be more appropriate
How do we examine the vagina and what do we look for? (2)
Digital, Speculum or Endoscopic examination of vagina and cervix
- Confirmation of normality and estimation of stage of the cycle
- Evidence of gross pathology
–e.g. Presence of persistent hymen
–e.g. Evidence of disease such as vaginitis or cervicitis
–e.g. Evidence of trauma including scaring or deformation of cervix
–e.g. Pooling of urine or pus in the vagina
What can be seen on the below pictures:

A) Dioestrus – cervix hard and narrow
B) Oestrus – cervix large and oedematous
C) Cervicitis
D) Cervical adhesions
What is seen on rectal exam of mare? (4)
- Confirmation of normality
- Confirmation of cyclicity and stage of cycle
- Confirmation of non-pregnancy
- Evidence of gross pathology
–e.g. Absence of, or large uterus
–e.g. Inactive ovaries, or large ovaries
What are the 2 possile reasons for 2 small ovaires?
. Mare is acyclical
- Anoestrus (cervix/uterus will be intermediate in size/tone)
- Prepubertal (cervix/uterus will be intermediate in size/tone)
- Mare is abnormal (e.g. Turners Syndrome) (all tubular genitalia are small)