3 - GI Presentations Flashcards
What organs cause acute abdominal pain in each of the four quadrants, the epigastrium and the suprapubic area?
Also consider lungs, cardiac, testicular and gynaecological pathologies, DKA

What is an acute abdomen and how do you assess a patient with this?
Sudden onset of severe abdominal pain
Need to decide if patient is critically unwell and needs surgical intervention so check observations and observe patient from bed with ABCDE
What are some causes of acute abdomen that require immediate urgent intervention?
- Intraabdominal bleeding
- Perforated viscus
- Ischaemic bowel

Intraabdominal bleeding is a pathology that presents as acute abdomen and requires urgent intervention as it can cause hypovolemic shock. What are some causes of this type of bleeding and how will a patient present with this?
- Ruptured AAA
- Ruptured ectopic pregnancy
- Bleeding gastric ulcer
- Trauma.
- Hypovolemic shock: tachycardia, hypotensive, cold to touch, clammy and pale

A perforated viscus is a pathology that presents as acute abdomen and requires urgent intervention as it causes peritonitis. What are some causes of this and how will a patient present with this?
- Peptic ulceration
- Small or large bowel obstruction
- Diverticular disease
- IBD
Patients will lay completely still with generalised peritonitis (unlike renal colic where they will be moving to get comfortable)

Ischameic bowel (Acute Mesenteric Ischaemia) is a cause of acute abdomen that requires urgent surgical intervention. How will this present in a patient and how is it diagnosed?
Severe pain out of proportion to clinical signs has ichaemic bowel until proven otherwise
Exam often remarkable but diffuse constant pain. Often acidaemic, have a raised lactate and are physiologically compromised
Definitive diagnoses via CT with IV contrast

How does colic present?
Pain that crescendos to become very severe and then goes away completely
e.g biliary colic, ureteric colic, and bowel obstruction.
What is peritonism?
Localised inflammation of the peritoneum, usually due to inflammation of a viscus that then irritates the visceral then parietal peritoneum
Pain starts in one place (visceral) then moves to another place/becomes generalised (parietal)
e.g appendicitis
What labatory tests and imaging should you do for all cases of acute abdomen?
Lab Tests
- Urine dipstick ±MC&S: check for signs of infection, haematuria, pregnancy
- ABG: for bleeding or septic patients. Look at O2, rapid Hb, lactate to see perfusion of organs
- Routine bloods: FBC, U&Es, LFTs, CRP, amylase and a group and save if likely to need surgery soon
Imaging
- eCXR: for pneumoperitoneum or lower lobe lung pathology
- US: see image
- CT
- ECG: to rule out cardiac pathology causing referred pain

What may a raised serum amylase level mean in a patient with acute abdomen?
- 3x normal limit: pancreatitis
- Raised but not 3x: perforated bowel, ectopic pregnancy, or diabetic ketoacidosis (DKA)
How is acute abdomen managed generally before a diagnosis is made?
- IV access +/- fluids
- Nil by mouth
- Analgesics
- Antiemetics
- Initial imaging, bloods and urine dip
- VTE prophylaxis
- Consider NG tube and catheter if unwell to monitor fluid balance

What are the key principles of making surgical incisions?
- Incisions should follow Langer’s lines where possible, for maximal wound strength with minimal scarring
- Muscles should be split and not cut (where possible)

What are the incisions used for an appendectomy?
Made at McBurney’s point (2/3 from umbilicus to ASIS). Passes through passing through all of the abdominal muscles, transversalis fascia, and then the peritoneum to the abdominal cavity
Lanz Incision: transverse incision that follows Langer lines so more aesthetically pleasing and less scarring
Gridiron incision: oblique (superolateral to inferomedial)

What are the names of the following incisions?

- Midline
- Paramedian
- Kocher
- Chevron / rooftop incision or modification
- Mercedes Benz incision or modification
What is a midline incision used for?
Anywhere from the xiphoid process to the pubic symphysis, passing around the umbilicus
Will cut through skin, subcutaneous tissue, fascia, linea alba and tranversalis fascia, peritoneum before reaching the abdominal cavity
Can be used for emergency procedures as good visualisation. Also minimal blood loss and nerve damage. However bad scarring

What is a paramedian incision?
Rarely used but when used it is to get to lateral viscera like kidneys and spleen
2-5cm lateral to the midline, anterior rectus sheath is separated and moved laterally, before the excision is continued through the posterior rectus sheath (if above the arcuate line) and the transversalis fascia, reaching the peritoneum and abdominal cavity
Takes a long time but prevents division of rectus muscle. However can damage lateral muscle blood and nerve supply causing atrophy of muscle medially

What is a Kocher incision and what is it used to gain access to?
Subcostal incision used to gain access to gall bladder for the biliary tree.
Runs parallel to the costal margin, starting below the xiphoid and extending laterally.
Pass through all the rectus sheath and rectus muscles, internal oblique and transversus abdominus, before passing through the transversalis fascia and then peritoneum to enter the abdominal cavity.
Heals well
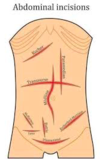
What are two modifications of the Kocher incision and what are they used for?
Chevron / rooftop incision
- Extension of Kosher to the other side
- May be used for oesophagectomy, gastrectomy, bilateral adrenalectomy, hepatic resections, or liver transplantation
Mercedes Benz incision
- Liver transplantation

What laparoscopic port site is almost always the same in every surgery?
Umbilicus for camera port
Common instruments include camera, cutting and dissecting scissors, and grippers
What are some of the causes of haematemesis?
Emergency (due to haemorraghe)
- Oesophageal varices: often due to portal hypertension from alcohol abuse. Needs urgent OGD
- Gastric ulceration: erosion into blood vessels, usually lesser curve of stomach and posterior duodenum. May have history of epigastric pain, NSAIDs, H.Pylori
Non-emergency
- Mallory-Weiss Tear: just needs reassurance and monitoring. If severe or prolonged this warrants OGD
- Oesophagitis: due to GORD, infections such as candidiasis, radiotherapy, Crohn’s, ingestion of toxic substances
- Gastritis, Gastric malignancy, Meckel’s diverticulum

When a patient presents with haematemesis, what do you need to find out in the history?

See image but also check for peritonism, epigastric tenderness, evidence of underlying cause e.g liver stigmata

What investigations are done when a patient has haematemesis?
- Routine bloods (FBC, U&Es, LFTs, and clotting) and VBG
- Group and Save and crossmatch 4 units of blood
- OGD is definitive, within 12 hours
- Erect CXR if suspect perforated peptic ulcer
- CT abdomen with IV contrast if too unwell for OGD or if OGD is unremarkable

What is the Glasgow-Blatchford Bleeding Score?
Decide whether Upper GI bleed can be managed as outpatient or inpatient with endoscopy
Rockall Score (severity score for GI bleeding post-endoscopy)
What is the best imaging for acute abdomen and haematemesis?
Acute Abdomen: CT with IV contrast
Haematemesis: OGD
How is haematemesis due to peptic ulcer disease and oesophageal varices managed?
- Initial: 2 large bore IV cannulas, start fluid resuscitation if needed, and crossmatch blood
Endoscopy:
- Peptic ulcer disease: Injection of adrenaline and cauterisation or embolisation of gastroduodenal artery. High dose IV PPI +/- eradication therapy
- Oesophageal varices: prophylactic antibiotics and Terlipressin.
Endoscopic banding, Somatostatin analogues (e.g. octreotide) or vasopressors (e.g. terlipressin), Long-term repeated banding and long term beta blockers
What is the aetiology of dysphagia and what are some questions you should ask someone with this?
- Is there difficulty in initiating the swallowing action?
- Do you cough after swallowing?
- Do you have to swallow a few times to get the food to pass your throat?
Ask about regurgitation, the sensation of food becoming ‘stuck’, hoarse voice, weight loss, referred ear or neck pain

How is a dysphagia presentation investigated?
- URGENT OGD and biopsy to rule out malignancy
- FBC
If endoscopy normal can arrange manometry and 24hr pH studies to look for motilitity disorders, or barium swallow to look for pharyngeal pouch

How is dysphagia managed?
- Treat underlying cause e.g excision/palliation for malignancy
- Involve speech therapists and dieticians early if ongoing
What is a closed loop obstruction?

Why is urgent fluid resuscitation required in a bowel obstruction?
Once the bowel segment has become occluded, dilatation of the proximal limb of bowel occurs, resulting in an increased peristalsis of the bowel.
This leads to secretion of large volumes of electrolyte-rich fluid into the bowel (often termed ‘third spacing’).
What is the aetiology of small and large bowel obstructions?
Small bowel – adhesions and hernia
Large bowel – malignancy, diverticular disease, and volvulus
SURGICAL SIEVE: outside, within the wall, within the lumen

What are some clinical features of a bowel obstruction?
- See image for features
- Examination: abdominal distension, focal tenderness, tinkling bowel sounds on auscultation, tympanic sound on percussion
- Patients develop guarding and rebound tenderness with abdominal tenderness when ischaemia of the bowel is starting

What are some differential diagnoses for bowel obstruction?
- Pseudo-obstruction
- Paralytic ileus
- Toxic megacolon
- Constipation
What investigations are done if you suspect a bowel obstruction?
- Urgent bloods and a G+S due to third spacing
- VBG to look for raised lactate (ischaemia) or metabolic derangement due to vomiting/dehydration
- CT with IV contrast is imaging of choice
- AXR
- Water soluble contrast study (gastrograffin) in small bowel obstruction from adhesions from surgery

Why is CT imaging better than AXR for bowel obstructions?
(1) more sensitive
(2) can differentiate between mechanical obstruction and pseudo-obstruction
(3) can find site and cause of obstruction so good for operative planning
(4) presence of metastases if caused by a malignancy
What would you see on an AXR of a bowel obstruction?


How is a bowel obstruction managed conservatively?
- If closed loop or signs of ischaemia need urgent surgery
- If no signs of ischaemia DRIP AND SUCK (see image)
- Water soluble contrast study if does not resolve within 24 hours conservative management.

What is the surgical management of a bowel obstruction?
- Indications of surgery (see image) plus virgin abdomen
- Laparotomy
- Resection of bowel if ischaemic and anastomose or stoma

What are some complications of bowel obstruction?
- Bowel ischaemia
- Bowel perforation leading to faecal peritonitis (high mortality)
- Dehydration and renal impairment
What is a red flag that ischaemia may be developing in a suspected bowel obstruction?
- Colicky pain that becomes constant in nature or worse on movement
- Guarding and rebound tenderness





































