Advanced Immunity, Inflammation & Infection + Advanced Special Groups Flashcards
(23 cards)
What are the TWO main categories of changes that happen to the body during surgery?
Hormonal –> Corticotrophin (ACTH) levels increase (increasing cortisol), and growth hormones inhibits glucose uptake/use whilst insulin secretions are decreased, so blood glucose will raise (hence the need for sliding scales)
The thyroid also has an increased activity, increasing the body temperature
Metabolic –> An increase in catabolic (breaking down) enzymes, meaning there’s an increase in glucose, AAs and fatty acids
Water and electrolyte levels are also often disturbed
What is the Triad of anaesthesia?
And what drugs would be used pre-op and peri-operatively?
Analgesia, Amnesia and Muscle Relaxant
Pre-op –> Anxiolytics (midazolam), antibiotics (broad spectrum), steroids and GI protection
Peri-op –> Propofol/Thiopental or gas with O2/N2O mix for induction)
Opitates, propofol IV (not in those with egg allergies) and O2/N2O mix gas (maintenance)
Switch to Oxygen, neostigmine (muscle relaxant) and anti-cholinergenics like atropine (end)
For most surgeries, what would you do if the patient was on the following medication?
Anticoagulants
Anti-platelets
Cardiac meds
Steroids
Insulin
Oral Contraceptives
Tamoxifen
MAOIs
Lithium
Anticoagulants –> Wafarin (stop 5 days before) and DOACs (2 days before)
Anti-platelets –> Stop 2 days before
Cardiac meds –> Stop unless they’re protective for other reasons
Steroids –> Keep
Insulin –> Can give long acting in the morning, but then put on a sliding scale (oral hypoglycaemics are okay)
Oral Contraceptives –> Hold (but dependent on the patient)
Tamoxifen –> Continue
MAOIs –> Dependent on what it’s being used
Lithium –> Keep
What are the following procedures?
Apendictectomy
Hemi-colectomy
Para-thyroidectomy
Oophorectomy
Laprotomy
Laproscopy
Apendictectomy –> removal of the appendix
Hemi-colectomy –> removal of half of the colon
Para-thyroidectomy –> removal of the parathyroid gland
Oophorectomy –> removal of the ovaries
Laprotomy –> open the front of the GI tract
Laproscopy –> same as above but not opening, using instruments and cameras instead
What are the 4 main things that occur as a result of Sepsis, which make it so severe?
Hypovolaemia
Hypoperfusion at a cellular level
Cell Death
Organ Dysfunction
All this is due to the inflammatory response that is produced from the causative agent
What are the 9 Red Flags of Sepsis?
AVPU of V, P or U (so not too with it)
Acute confusion
RR over 25 per min
Needs oxygen to keep sats above 92%
HR over 130 per min
Systolic BP under 90mmHg (or a drop of 40 from normal)
Not passed urine in the last 18hrs
Non-blanching rash
Recent chemotherapy (last 6 weeks)

What are the Sepsis 6?

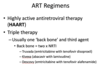
What is an ART regime?
Triple therapy used to treat HIV
Contains two NRTIs (non-reverse transcriptase inhibitors), known as the backbone, and a third drug
What is Tenofovir Alafenamide (TAF)?
A salt of tenofovir (an NRTI) with increased solubility and reduced side effects
This is ideal as the drug is nephrotoxic, so we want to give as little as possible

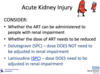
Does Lamivudine (an NRTI) need to be dose adjusted in an AKI?
YES
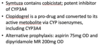
Which drug, given after a TIA, is most problematic when the patient is on HIV treatment?
Clopidogrel
This is because it’s a pro-drug that is metabolised by CYP enzymes, which will effect the levels of most HIV drugs!
If Dolutegravir (a protease inhibitor) is given to patient whilst being treated for TB and HIV, what should be done to the dose?
Dose should be increased by 50% due to the AUC being decreased by the TB treatment (usually change from 50mg OD –> BD)
Important to not alter the TB treatment, but the HIV treatment instead!
What’s the difference between PEP and PrEP?
PEP –> Post Exposure Prophylaxis
A 28 day course of drugs taken after exposure to prevent HIV. Can’t have 48hrs between doses as then the entire regimen won’t work
PrEP –> Pre-Exposure Prophylaxis
ART therapy that can be taken daily (like the pill). Shouldn’t be given if you have HepB, as it increases liklihood of sex without a condom (riskier sex)
What is the ‘mismatch’ for this patient wanting to get a kindey transplant?

1-0-2
1 –> From A
0 –> From B
2 –> From DR

What is the main ‘induction agent’ for immunosuppresion for kidney transplants?
Why are the other 2 possible agents not often used?
Basiliximab (IL-2 inhibitor)
Binds and inhibits IL-2 on T cells
20mg given 2 hours prior to surgery, and then 20mg 4 hours after
Cant use Almetuzumab or ATG as they can only be used once due to the body creating antibodies against them!
What are Calcineurin Inhibitors (CNI’s)?
Tacrolimus (1st line) and Ciclosporin –> Used for maintainence immunosuppresion
These inhibit calcineurin activity, thus preventing T cell proliferation
These have specific brands! You cannot switch them!
Tacrolimus –> Needs to be given on an empty stomach, and is metabolised in the gut so D+V will increase active levels
Levels are increased by macrolides and decreased by rifampicin
Ciclosporin –> Should be diluted with juice or squash before administration due to horrible taste

Which form of Mycophenolate Mofetil is the pro-drug form?
Mycophenolate sodium
Mycophenolate acid is the enteric coated version (so needs less than Mofetil, with a conversion ratio of acid 720mg : 1g Mofetil)

What 3 types of prophylaxis is given to high risk patients after kidney transplants?
PCP Prophylaxis –> Co-trimoxazole
CMV Prophylaxis –> Aciclovir and Valganciclovir
TB Prophylaxis –> Isoniazid and Pyridoxine
What are the 2 main interventions that are done when a kidney is rejected?
Pulsed methylprednisolone
ATG is given –> Which causes a cytokine storm
Should be given with hydrocortisone and chlorphenamine

In RA, why would we want to taper people off of drugs that have got them into remission?
Cost
Side Effects
Convienience (mabs can be hard to store and administer)
Prevent cummulative toxicity
In RA, what was found when comparing biologics treatment cessation and treatment tapering?
Stopping is worse than continuing the drug
Tapering off is probably just as good as continuing the drug….so you might as well do that! (But this is dependent on the patient)
The deeper/longer the patient is in remission for, the less likely they are to flare up when the dose is reduced
What are the 7 most common signs of sepsis?
High/low temperature
Slurred speach/confusion
Extreme shivering/muscle pain
Passing no urine in a day
Severe breathlessness (blue lips)
“I feel like I might die” –> Feeling dreadful
Skin mottled or discolured
In RA, why is dose optimisation at an inappropriate time a bad idea?
As it cause an RA flare
This makes getting control of the the RA afterwards much harder


