Chronic pain, brain anatomy, signalling in the NS Flashcards
(172 cards)
Which lobe is the precentral gyrus part of?
Frontal
What lobe is the postcentral gyrus part off?
Parietal
Where is Broca’s area?
On the inferior frontal gyrus
Which hemisphere is Broca’s more commonly found in?
The left
Which gyri is the auditory complex found on?
Superior temporal gyri
What is the function of Broca’s area?
Motor aspect of speech - speech associated gestures
What does damage to Broca’s area do?
Expressive aphasia- non-fluent and slow speech
Where is wernicke’s area found?
Within the auditory association cortex
What is the function of Wernicke’s?
Sensory language areas, lexical processing
What can damage to Wernicke’s area cause?
Receptive aphasia - extremely poor comprehension
What are the most anterior and posterior parts of the corpus callosum called?
Genu (anterior)
Splenium (posterior)
What is the rostrum of the corpus callosum?
The part that projects inferiorly and posteriorly from the Genu
Where is CSF made?
Choroid plexus within the ventricular system of the brain
How much CSF is produced per day, and what happens to it when it’s been used?
500ml produced per day 140ml circulates through the subarachnoid space
Reabsorbed into the venous drainage system
What is the function of CSF?
Affords mechanical and immunological protection to the brain and spinal cord
How does CSF pass from the lateral ventricles to the third ventricle?
Interventricular foramen
How does CSF pass from the third ventricle to the fourth ventricle?
Through the aqueduct of midbrain
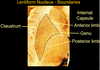
Which structures make up the lentiform nucleus?
Putamen
Globus palidus
What are the three borders of the lentiform nucleus?
Claustrum
Anterior limb
Posterior limb
Which motor axons pass by the Genu of the lentiform nucleus?
Corticobulbar axons
Which axons pass by the posterior boundary of the lentiform nucleus?
Corticospinal axons
What are the three main pairs of arteries given off by the circle of Willis?
Anterior cerebral arteries
Middle cerebral arteries
Posterior cerebral arteries
Roughly what areas of the brain does the anterior, middle and posterior cerebral arteries supply?
Anterior - frontal and parietal
Middle - temporal
Posterior - occipital
Which eight, fused bones make up the cranial cavity?
Frontal
Occipital
Sphenoid
Ethmoid
2 x parietal
2 x temporal